A 5-year-old castrated male American Shorthair cat weighing 5 kg was exposed to its owner’s topical minoxidil when it accidentally knocked over the solution bottle, thereby spilling it onto its body and licking it. The cat subsequently presented with acute lethargy and anorexia and showed no signs of urination. Consequently, the cat presented to the SMART animal hospital Sinsa 24 h after the minoxidil exposure. On physical examination, it exhibited rapid and shallow breathing (respiratory rate: 60 breaths/min) and pale mucous membranes. The cat also presented with signs of hypothermia (rectal temperature: 36.3 °C), along with mild tachycardia (204 beats/min; reference range: 100–140 beats/min) and hypotension (systolic blood pressure: 80 mmHg; reference range: 90–140 mmHg; Doppler method).
The complete blood count was within the reference interval. Serum biochemistry revealed an elevated blood urea nitrogen level of 44 mg/dL (reference range: 16–36 mg/dL), hyponatremia (146 mmol/L; reference range: 149–157 mmol/L), and hypochloremia (106 mmol/L; reference range: 117–127 mmol/L). Thoracic radiography revealed a mild bronchointerstitial pulmonary pattern and retraction of the caudal lung lobes from the thoracic wall (
Figure 1). Based on the cat’s history and previous annual check-up results, including normal pro-BNP levels and no abnormalities in chest radiographs, a provisional diagnosis of minoxidil toxicosis was made.
The cat was hospitalized in the intensive care unit with heated pads used to help restore the cat’s normal body temperature and received oxygen therapy and intravenous fluids. Furosemide (1 mg/kg; Lasix, Handok Inc., Seoul, Republic of Korea) was intravenously administered to alleviate pleural effusion. A continuous rate infusion (CRI) of dopamine (Huons Dopamine Inj., Huons, Seongnam, Republic of Korea) was administered at a rate of 5 μg/kg/min to improve hypotension and increased to 10 μg/kg/min. Despite treatment, the cat’s clinical symptoms did not improve, and its blood pressure decreased to 70 mmHg. Hemodialysis was initiated on the second day of hospitalization with the owner’s consent. Intermittent hemodialysis (IHD) sessions were performed using a Fresenius multifiltrate system (Fresenius Medical Care AG & Co. KGaA, Bad Homburg, Germany) using polysulfone dialyzers (Ultraflux
® AV paed, Fresenius Medical Care AG & Co. KGaA, Bad Homburg, Germany) and the pediatric continuous venovenous hemodialysis (CVVHD) mode. Under sedation with propofol (Provive Inj., Pharmbio Korea Inc., Seoul, Republic of Korea) at CRI of 0.2 mg/kg/min, vascular access via the right jugular vein was obtained using an 8 Fr-sized 2-lumen central venous catheter set (Blue FlexTip
® ARROWgard
® Blue catheter, Arrow international, Inc., Cleveland, OH, USA). Butorphanol (Butorphan Injection, Myungmoon Pharm, Seoul, Republic of Korea) was prescribed for analgesia as needed. The average blood flow rate was 25 mL/min, and the dialysate flow rate was maintained at 500 mL/h during each 4 or 5 h session. The amounts of blood processed were 1.2 and 1.5 L/kg in the 4 and 5 h sessions, respectively. MultiBic
® dialysate (Fresenius Medical Care Deutschland GmbH, Wendel, Germany) was used, and ultrafiltration was carefully performed to reduce the patient’s fluid retention caused by intoxication. The target dry weight was 4.7 kg, and the ultrafiltration rate was initially 5 mL/h and gradually increased to 25 mL/h. To prevent unstable hemodynamic changes, such as decreasing blood pressure, 40 mL of type A feline blood was primed for an extracorporeal circuit before each session. After two sessions of IHD over 2 consecutive days, the cat showed a slight improvement in overall condition and appetite. As the body temperature and blood pressure returned to the normal range, the dopamine CRI was tapered and discontinued (
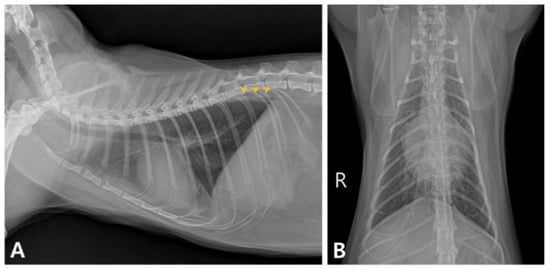
Supplementary Figure S1). Pleural effusion was still evident on chest radiography (
Figure 2A,B), and echocardiography revealed right ventricular dilatation, tricuspid regurgitation, and a small amount of pericardial effusion (
Figure 3). To resolve these issues, the cat’s treatment plan was adjusted to include furosemide CRI at a rate of 0.5 mg/kg/h and oral pimobendan (1.25 mg/cat q12h; Vetmedin, Boehringer Ingelheim, Ingelheim, Germany) and spironolactone (1 mg/kg q12h; Spiracton Tab, Daewon Pharmaceutical, Seoul, Republic of Korea). The cat’s respiratory pattern gradually improved, and follow-up radiography demonstrated a reduction in pleural effusion (
Figure 2C,D). The furosemide CRI was gradually reduced and changed to oral medication 5 days after the second IHD session. The cat eventually recovered fully and was discharged on the 11th day of hospitalization. Follow-up blood tests and thoracic radiography conducted 7 days after discharge showed no abnormal findings.
Source link
Woonchan Ahn www.mdpi.com