1. Introduction
China has the world’s largest older population and is one of the fastest-aging countries [
1]. Aging is associated with significantly increased vulnerability in both physical and psychological health, making elderly individuals highly susceptible to various diseases [
2].
The Healthy China Action 2019–2030 illustrated that 180 million older adults in China have chronic diseases, accounting for 75% of the older population in China [
3]. Deaths from chronic diseases occupy 86.6% of total deaths in China, while disease burden (the pressure on the overall socio-economic and health of society) exceeds 70% of the total burden [
4]. Therefore, it is imperative that the health status of older adults suffering from chronic conditions receive substantial attention.
‘Older population’ has a different definition in different countries. In China, it usually refers to residents who are older than 60 years old [
3]. Activities of Daily Living (ADL), an important indicator for appraising the health status of older adults, are instrumental in evaluating the deterioration of daily physical functions [
5]. ADL include using restrooms, eating, dressing, grooming, walking, and bathing. An ADL disability denotes an individual’s incapacity to autonomously perform fundamental tasks, resulting in repercussions for the individual and their family and society at large [
6]. Studies reported that chronic diseases heighten the likelihood of ADL impairment in older adults, attributable to characteristics such as protracted illness duration, gradual recuperation, heightened vulnerability to complications, and the presence of potential risk factors associated with functional disability. As a result, older adults with chronic diseases have a higher prevalence of ADL disability [
7,
8,
9]. ADL disability transition refers to a change in an individual’s incapacity to autonomously perform fundamental tasks, which may involve the worsening, recovery, or improvement of ADL.
A number of studies analyzed the patterns of ADL disability transitions, while most of them focused on the situation between two states (with and without ADL disability) [
10,
11,
12]. However, the occurrence of ADL disability is a dynamic and progressive process [
13]. The multi-state Markov model, a tool for dealing with longitudinal data, is capable of the continuous dynamic of stochastic processes, including the transitions among multiple different ADL disability states [
14]. Furthermore, it can simultaneously consider all states, outcomes, and timing of transitions between states and dynamically evaluate the progression of diseases [
15]. Various factors impact ADL disability incidence, such as sex, age, institutional contexts, education, marital status, and social activities [
13]. However, limited research exists on factors affecting transitions between ADL disability states.
The current study constructed a multi-state Markov model and adopted a retrospective cohort study design to analyze the patterns and factors of mutual transitions between multiple different ADL disability states in older adults with chronic diseases.
2. Methods
2.1. Study Population
Shanghai Elderly Care Unified Needs Assessment (SECUNA) dataset was used in the present study. SECUNA is a longitudinal follow-up conducted in Shanghai (China) from 2013 to 2021. SECUNA was designed to investigate the long-term care needs of older adults, including those in the community and various institutions. The current study used 2014, 2015, 2016, and 2017 data, with 2014 as the baseline. The inclusion criteria included (1) age ≥ 60 years old; (2) chronic diseases throughout 4 years (both new and pre-existing cases included); (3) investigated by SECUNA at least twice. The exclusion criteria were (1) deceased participants and (2) missing data on chronic diseases, ADL, or any covariates.
2.2. Outcome Measurement
ADL was assessed with a 20-item self-design scale, totaling 20 points (See
Appendix A,
Table A1), adapted from Lawton and Brody’s 1969 scale [
16]. The points for each item ranged from 0 to 1. Points from the 20 items were summed to calculate the participants’ total ADL points. A point of 20 being no ADL disability, a point range from 8 to 20 (excluding 20) being mild ADL disability, and a point range from 0 to 8 (excluding 8) being severe ADL disability.
2.3. Chronic Disease Situation
SECUNA listed ten chronic diseases: diabetes, hypertension, chronic obstructive pulmonary disease, chronic pneumonia, Parkinson’s disease, cerebral hemorrhage, advanced tumors, coronary atherosclerotic heart disease, cerebral infarction, and fractures of the lower limbs. Investigators assessed each condition, confirmed by family doctors and medical records for quality control.
2.4. Covariates
We used covariates to determine which factors influenced transitions between different ADL disability states in older adults with chronic diseases. The socio-demographic information included age, sex, and educational level. The educational level was classified as illiteracy, primary school, middle school, high school, and college or higher level.
The place of residence was divided into two categories: living at home (including freehold houses, private houses, and various types of rented houses) and institutions for older adults (including nursing homes, care and attention homes, community health service centers, and hospitals). The economic sources were classified by the existence of a stable pension (with pensions; /without pensions and need for family, friends, or other allowances). The co-morbidity group included older patients with two or more chronic diseases.
2.5. Statistical Analysis
Participant baseline characteristics were described using frequency and composition ratios. The multi-state Markov model in this study comprised three interconvertible states: no ADL disability, mild ADL disability, and severe ADL disability, with no absorbing state due to a low mortality rate. An absorbing state describes a state where, once you enter it, you cannot leave. It is a way to model situations where something reaches an end state and cannot go back to how it was before. In the current study, the absorbing state means death.
Following the calculation of ADL disability state transition frequency in older adults with chronic disease over four years, we estimated transition intensity (
) between states and the one-year transition probability. Transition intensity measures the speed at which things change from state to state in a Markov model. The higher the intensity, the faster the transition can happen, and the lower it is, the slower the transition will be.
describes the instantaneous risk of moving from state r to state s at time t, while the one-year transition probability represents the likelihood that an individual in state
r at time
t will be in state s one year later.
In addition, the effects of covariates on a particular transition intensity were estimated by modeling the intensity as a function of these variables, similar to a proportional hazards model [
17]. Proportional hazards model takes survival outcome and survival time as dependent variables and can simultaneously analyze the impact of numerous factors on survival period [
18].
We estimated the effects of covariates on six transition scenarios, with age modeled as a continuous variable and education level as an ordered categorical variable. Meanwhile, sex, place of residence, economic source, and chronic disease grouping are grouped as unordered categorical variables. A detailed explanation of the model has been reported in previous studies [
17,
19].
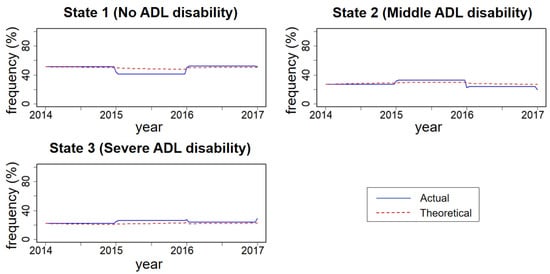
Descriptive statistics of baseline characteristics were conducted using IBM SPSS 25.0 [
20]. The multi-state Markov model was developed using the MSM package in R 4.3.2 [
19]. The plot function of R 4.3.2 was utilized to illustrate actual and theoretical frequency percentage curves for each state, evaluating the fit of the multi-state Markov model [
21].
4. Discussion
The study investigated transition patterns between three ADL disability states in older adults with chronic diseases. Those with mild ADL disability were more likely to experience improvement rather than deterioration, while those with severe ADL disability were more likely to remain where they were than show improvement. Among six transition scenarios, place of residence was associated with four, age and economic sources with three, and sex with two, and educational level and chronic diseases grouping were associated with one transition scenario.
Based on transition frequency, estimated intensity, and predicted probability, transitions in ADL disability states (improvement, non-change, or worsening) are consistently observed in older adults with chronic diseases, aligning with prior research [
22,
23,
24]. This suggests that the development of disability in old age is not unidirectional—it can both gradually deteriorate and potentially improve over time. Hence, nursing interventions and other strategies should aim to improve ADL states and enhance older adults’ quality of life. Studies have demonstrated the feasibility of strengthening exercise, nutrition, cognition, and social support [
25,
26,
27,
28,
29].
However, among older adults with chronic diseases, state transitions were not the same for those with different ADL disability states, which makes nursing interventions more complex. In terms of transition intensity and one-year transition probability, older adults with mild ADL disability are more likely to improve rather than deteriorate. Proactive measures are needed to enhance support for maximizing positive change. Similar to a previous study [
30], older adults with severe ADL disability face challenges in improving their state. They need comprehensive medical care, social support, and family care to cope with the mixed pressures of chronic diseases and disability. Older adults without ADL disability, although less likely to experience worsening, still have a probability of transitioning to severe disability within one year, according to the transition probability. This highlights the need for early prevention and regular health monitoring. Medical facilities and nursing homes should implement targeted preventive healthcare strategies to manage the health of older adults with chronic diseases effectively, focusing on improving their quality of life and reducing unnecessary medical costs.
The present study tested the impacts of several factors on the transition of ADL disability state in older adults with chronic diseases. Consistent with previous studies [
31,
32], increasing age correlated with decreased physical function in older adults, elevated risk of transitioning to mild and severe ADL disability, and reduced likelihood of improvement in ADL disability. Prior research indicated males were more likely to improve from ADL disability than females [
33,
34]. In our study, this trend was evident transitioning from severe to mild disability only. Another study indicated that males had higher rates of improvement in ADL disability than females at ages 50–65 and 90–100 [
35], suggesting a potential advantage for males, but detailed research is necessary. While many studies have shown a faster increase in disability among older adults with lower education, often from no ADL disability to having ADL disability [
36,
37], our study focused on a different scenario and found that older adults with lower education were at higher risk of worsening from mild to severe ADL disability. We found that older adults with no ADL disability in institutions had a lower risk of state deterioration, but the situation of those with ADL disability was not good. In institutions, older adults with middle ADL disability had a higher risk of state deterioration, and those with severe ADL disability had lower rates of state improvement. This may be because home care is China’s predominant mode of care [
38]. Older adults are only institutionalized when care needs exceed family capacity, diminishing recovery prospects. China’s introduction of long-term care in the past two decades has led to persisting issues in institutional care, leaving the long-term care needs of older adults with ADL disability unmet [
39]. A cohort study that focused on the income levels of older adults in the US and the UK showed that low-income individuals have a higher disability rate than high-income individuals [
40]. This is similar to the current study, where older adults without pensions are more likely to transition from no ADL disability to mild ADL disability. Consistent with previous studies, co-morbidity impedes improvement in ADL disability state in older adults, but the current study demonstrated this pattern in only one transition scenario. Based on the analysis of influencing factors using the Markov model, we can observe the situation of multi-state transition. We found that among the older adults with chronic diseases, the influencing factors for state transition in those with different ADL disabilities were not the same, which helped us to identify the high-risk group of ADL disability and carry out targeted prevention and treatment for this group to reduce the occurrence of ADL disability or to slow down the development process of ADL disability.
The multi-state Markov model analyzed the complex mutual transitions between ADL disability states, but its generalizability is limited by data processing intricacy and the need for programming in specific studies [
41]. Limited studies utilized a multi-state Markov model to examine ADL disability transitions in older Chinese adults. Research on transitional patterns between ADL states remains scarce in this population [
31,
42,
43]. In addition, we focus on a specific group of older adults with chronic diseases because they not only have a high ADL disability but also have a high demand for healthcare and long-term care. Due to the lack of long-term care insurance coverage, older adults with chronic diseases in China may tend to overuse medical services, ultimately leading to an increase in medical expenses [
44,
45]. Therefore, we focused on the transition patterns and influencing factors between different ADL disability states in older adults with chronic diseases, aiming to improve their quality of life and reduce medical burden. Furthermore, as a city with a high degree of aging, Shanghai’s research results provide valuable experience and inspiration for other regions, which will help formulate more accurate health policies for older adults nationwide. Meanwhile, by comparing with other regions, differences in ADL disability among different areas can be revealed, providing a scientific basis for further improving the elderly health service system. These studies are of great significance for promoting the development of global elderly health.
Several advantages and limitations remain in the present study. The current study adopted long-term monitoring and the Markov model to accurately assess transitions between various ADL disability states, distinguishing itself from prior studies focusing on specific times or states. Our findings aid in predicting ADL disability transitions in older adults with chronic illnesses, informing strategies for early prevention and interventions to maintain health.
As for the limitations, the mortality rate had not been reported, which may potentially bias transition outcomes. Secondly, the sample of the current study is limited to Shanghai residents, which may affect generalizability. Thirdly, factors related to the COVID-19 pandemic were not considered, as the current study used data from 2014 to 2017.
In the next step of our research, we plan to use more representative samples to observe the transition patterns of ADL disability in older adults with each chronic disease to draw more accurate conclusions and better propose response measures. In addition, for public health issues, epidemics are an important factor, so we will compare the sample differences before and after the epidemic to explore it in depth.
5. Conclusions
In summary, it is common for older adults with chronic diseases to have their ADL disability state unchanged or improved as well as deteriorated. However, the state transition patterns in those with different ADL disability states are not the same, and the influencing factors for state transition in those with different ADL disability states are also not the same.
State transitions among older adults with chronic diseases vary by ADL disability severity, with those having mild ADL disability showing greater potential for improvement, while those with severe ADL disability face significant challenges, underscoring the need for targeted, proactive interventions, comprehensive care, and early prevention strategies to enhance quality of life and reduce healthcare costs.
The results of this study are beneficial for relevant departments to adopt different preventive and health measures for those experiencing different ADL disability states among older adults with chronic diseases to strengthen health management, improve their quality of life, promote the rational allocation of long-term nursing service resources, and effectively respond to the social care needs brought about by aging.