1. Introduction
Obesity is a chronic and multifactorial disease characterized by a persistent imbalance in energy homeostasis [
1]. It has become a significant challenge for public health, tripling its prevalence worldwide over the last five decades [
2,
3]. Obesity is classified based on the body mass index (BMI) and metabolic status [
4], with obesity defined as BMI ≥ 30 kg/m
2 and overweight as BMI of 25–29.9 kg/m
2 [
5,
6]. Additionally, based on metabolic status, it is categorized into metabolically healthy obesity, metabolically abnormal obesity, or unhealthy obesity [
7,
8]. In addition to being a disease itself, obesity is a risk factor for all non-communicable chronic diseases and exacerbates some communicable diseases [
9,
10].
Environmental pollution, including air pollution, has been identified as a factor in the multifactorial causality of obesity due to the correlation observed between this condition and increased exposure to environmental pollutants [
11,
12]. In recent years, air pollution has been particularly concerning; it includes a complex mixture of particles and gasses with diverse chemical and physical compositions, originating from various sources and exhibiting spatial and temporal variability in toxicity [
13,
14]. Airborne particulate matter, especially fine particles ≤ 2.5 microns in diameter (PM
2.5), is generated by anthropogenic activities and natural sources. It adversely affects human health, ecosystems, and visibility and contributes to climate change [
15,
16].
The prevalence of obesity and air pollution from PM
2.5 have reached unprecedented levels [
17,
18]. In 2021, the World Health Organization (WHO) declared that air pollution is the leading global environmental health issue, prompting updated air quality guidelines recommending stricter limits on daily and annual exposure to PM
2.5 [
19]. Faced with this complex landscape, a study was conducted in a bioinformatics context using the Rothman causal model to analyze the impact of chronic PM
2.5 exposure on the etiology of metabolically abnormal obesity [
20]. Three new transcriptional signatures were reported: FAT-PM
2.5-CEJUS, FAT-PM
2.5-UP, and FAT-PM
2.5-DN. FAT refers to the Spanish acronym for transcriptional adipogenic signature, CEJUS refers to the Spanish acronym for “Justo Sierra” Study Center, UP refers to up-regulated, and DN refers to down-regulated. These signatures exhibited a transcriptional regulation profile in adipocytes that was statistically similar under high-fat diet (HFD) intake and chronic PM
2.5 exposure, affecting the peroxisome proliferator-activated receptor (PPAR) signaling pathway, small-molecule transport, adipogenesis gene pathway, cytokine–cytokine receptor interaction, and hypoxia-inducible factor 1 (HIF-1) signaling pathway [
20].
The PPAR signaling pathway plays a crucial role in regulating lipid metabolism and adipogenesis through its three subtypes: PPARα (PPAR alpha), PPAR-β/δ (PPAR beta/delta), and PPARγ (PPAR gamma) [
21,
22]. PPARα regulates the clearance of circulating lipids and gene expression related to lipid metabolism in the liver and skeletal muscle [
23,
24]. At the same time, PPAR-β/δ is involved in lipid oxidation and cell proliferation [
25,
26], and PPARγ promotes adipocyte differentiation and glucose uptake [
27,
28].
These receptors are activated upon binding specific lipid ligands, forming heterodimers with the retinoid X receptor (RXR) and binding to retinoic acid response elements (AREs) in target gene promoters, thereby modulating gene transcription [
29,
30]. Exposure to PM
2.5 significantly impacts this signaling pathway. In experimental mouse models, it has been shown that these particles inhibit the expression of PPARα and PPARγ in the liver. This inhibition is associated with negative regulation of these receptors and increased hepatic lipotoxicity [
31]. Additionally, functional studies have demonstrated that PM
2.5 induces adipogenesis by activating PPARγ in a 3T3-L1 preadipocyte differentiation model [
32].
The relationship between PPARs and obesity is reflected in their ability to regulate critical metabolic processes. In the context of obesity, PPARγ facilitates adipose-tissue formation, while PPARα and PPAR-β/δ influence lipid metabolism and metabolic health. The disruption of these pathways by PM
2.5 contributes to metabolic dysfunctions associated with obesity, as shown in recent studies [
27,
32].
The transport of small molecules is a biological pathway that includes various mechanisms. Among these are protein-mediated transport by the ATP-binding cassette (ABC) family and the assembly, remodeling, and clearance of plasma lipoproteins. The ABC transporter superfamily includes transmembrane proteins with diverse functions [
33,
34]. These proteins transport amino acids, lipids, inorganic ions, peptides, saccharides, metals, drugs, and proteins across cell membranes against concentration gradients, utilizing energy from ATP hydrolysis [
35,
36,
37]. Additionally, ABC transporters are involved in intracellular compartmental transport [
36,
38]. Protein-mediated transport by the ABC family through the ABCA7-1 complex is essential for moving phospholipids and cholesterol out of cells [
39,
40]. This complex forms on the cell surface, where apolipoprotein A-I (ApoA1) is an acceptor of phospholipids and cholesterol, while ABCA7-1 facilitates their export to the plasma membrane [
41,
42]. The formation of the ABCA7-1 complex is crucial for remodeling plasma lipoproteins and maintaining lipid homeostasis [
43,
44].
In the context of the assembly, remodeling, and clearance of plasma lipoproteins, three essential functions are recognized: lipid transport mediated by chylomicrons, the endocytosis and degradation of low-density lipoproteins (LDL), and lipid transport by high-density lipoproteins (HDL) [
45,
46]. These functions are divided into assembly, remodeling, and clearance processes. In chylomicron-mediated lipid transport, a reaction occurs where the chylomicron, with an outer coat of apolipoproteins A (ApoA) and C (ApoC), is converted into a chylomicron remnant [
47,
48]. This process is facilitated by the enzyme lipoprotein lipase (LPL), coactivated by apolipoproteins ApoA5 and ApoC [
49,
50]. LPL stimulates the hydrolysis of triglycerides (TG) present in the chylomicron, releasing long-chain fatty acids and diacylglycerols [
47,
51].
The adipogenesis gene pathway is essential for the differentiation process of preadipocytes into mature adipocytes and comprises various regulatory elements [
52,
53]. This pathway includes eight main categories: inhibitors of the transition to adipocytes, transcription factors (TF) and modulators, growth factors and hormones, markers of differentiated adipocytes, miscellaneous elements, insulin-action genes, potential lipodystrophy-associated genes, and adipocyte-secreted products [
54]. Among these elements, Pparα and CCAAT/enhancer-binding protein alpha (Cebpα) are key TFs in adipogenesis. Pparα (PPARα) and Cebpα (CEBPα) are essential for regulating genes that promote the differentiation of preadipocytes into adipocytes, playing crucial roles in lipid-metabolism regulation and adipose-tissue formation [
52].
Fibroblast growth factor 21 (FGF21) is a regulator of adipogenesis. In models of obesity and type 2 diabetes, FGF21 is an antidiabetic and lipid-lowering agent. The Forkhead box protein O1 (FoxO1) negatively regulates the expression of this gene through
PPARα in the liver [
55]. Additionally, the tet methylcytosine dioxygenase 2 (TET2), a protein that converts 5-methylcytosine (5mC) into 5-hydroxymethylcytosine (5hmC), participates in the epigenetic regulation of adipogenesis. The overexpression of
TET2 in adipocytes influences the regulation of genes such as
Cebpb,
Cebpa, and
Pparg, and its depletion in murine models inhibits adipocyte hypertrophy and protects against HFD-induced obesity [
56].
Exposure to PM
2.5 significantly alters the adipogenesis pathway. Studies with Nrf2
−/− mice showed that exposure to these particles decreases
PPARα and increases
PPARγ, suggesting a negative impact of PM
2.5 on the balance of these critical receptors for adipogenesis and lipid metabolism [
57]. Additionally, exposure of microglial cells to PM
2.5 revealed adverse effects, such as reduced cell viability and structural damage, with
Cebpa regulation mediated by differentially expressed long non-coding RNAs (lncRNAs) [
58].
The cytokine–cytokine receptor pathway is organized into eight main groups that regulate inflammation and metabolism: chemokines, class I helical cytokines, tumor necrosis factor (TNF) family, transforming growth factor-beta (TGF-β) family, class II helical cytokines, IL-1-like cytokines, IL-17-like cytokines, and other unclassified cytokines [
59]. These cytokines are soluble proteins or glycoproteins that act as essential regulators in immune and inflammatory processes, host adaptation, cell growth and differentiation, cell death, angiogenesis, and tissue repair to maintain homeostasis [
60,
61]. Cytokines exert their biological effects by binding to specific receptors on the surface of target cells. This binding activates intracellular signaling cascades that modulate gene expression and cellular responses [
62,
63]. The cytokine groups are subdivided into subgroups based on their structure and specific functions [
64,
65].
The role of heterogeneous nuclear ribonucleoprotein A1 (HNRNPA1) in lipid and glucose metabolism has been investigated. Obesity-related studies in mice have observed downregulation of the
Hnrnpa1 gene in white adipose tissue (WAT). This decrease in
Hnrnpa1 promotes greater macrophage infiltration and an increase in the expression of proinflammatory and fibrosis genes, exacerbating insulin sensitivity, glucose intolerance, and hepatic steatosis. Additionally,
Hnrnpa1 has been found to regulate the stability of
Ccl2 mRNA, and its inhibition improves inflammation in WAT and glucose homeostasis [
66]. Other studies have demonstrated that PM
2.5 directly influences inflammation in visceral adipose tissue, alters fat metabolism in the liver, and affects glucose metabolism in skeletal muscle through both CCR2-dependent and independent mechanisms [
67,
68].
Research conducted in humans explored various approaches to address metabolic health and obesity, revealing significant findings about the cytokine–cytokine receptor pathway. A randomized controlled study with 55 students examined the impact of moderate jogging on PM
2.5-induced high blood pressure. The results showed that this physical activity increased the levels of IL-6 and the myokine clustering and significantly reduced systolic blood pressure and inflammatory markers compared to the control group [
69]. Another study investigated the effect of calorie restriction on walking speed, considering BMI and plasma IL-6 levels. This study found that while calorie restriction improved walking speed, especially in individuals with obesity and high IL-6 levels, the reduction in BMI was the main factor for this improvement, and changes in IL-6 levels did not significantly impact walking speed [
70].
A study in Romania identified genetic loci associated with obesity. It found that 34.6% of adults were overweight and 31.4% were obese, with a high prevalence of cardiometabolic complications. This study revealed that the AG genotypes of the leptin (LEP) A-2548G polymorphism and the AA genotypes of the fat-mass and obesity-associated protein (
FTO) rs9939609 polymorphism were associated with a higher risk of obesity. Additionally, the GRGMLA haplotype might be a susceptibility factor for obesity, with significant associations between
LEP and leptin receptor (
LEP-R),
LEP and ghrelin (
GHRL), and
GHRL and
FTO [
71]. Another study examined DNA methylation levels in the nuclear respiratory factor 1 (
NRF1),
FTO, and
LEPR genes in the saliva of children. The study revealed that overweight or obese Euro-American children had higher methylation in
NRF1 and
FTO. In contrast, in African-American children, higher methylation of the
LEPR gene was associated with average weight and showed a negative relationship with obesity measures [
72].
The HIF-1 signaling pathway is a cellular mechanism activated in response to hypoxia. HIF-1 is a TF that regulates the expression of various genes involved in cellular adaptation to hypoxia [
73,
74]. This signaling begins with stabilizing and activating the HIF-1 complex, composed of the HIF-1α and HIF-1β subunits. The former is inducible, while the latter is constitutively expressed [
73,
75]. In normoxia, HIF-1α undergoes hydroxylation at specific proline residues, leading to its ubiquitination and subsequent degradation by the enzyme prolyl hydroxylase [
73,
76].
In the presence of hypoxia or other stimuli, such as nitric oxide or various growth factors, IL-6 binds to the IL-6R receptor on the cell surface, forming an active signaling complex [
77,
78]. This complex triggers an intracellular signaling cascade that activates STAT proteins, which induce the expression of the
Hif1a gene, encoding the HIF-1α subunit [
79,
80]. The activity of PHD is reduced, thereby stabilizing HIF-1α, which then interacts with coactivators such as p300/CBP to modulate its transcriptional activity [
81,
82].
Under hypoxic conditions, the HIF-1α subunit translocates to the nucleus, where it binds to HIF-1β to form the active HIF-1 complex [
75,
83]. This complex acts as a transcription factor that binds to specific DNA sequences known as hypoxia-response elements (HREs), located in the promoter regions of genes encoding proteins involved in the hypoxic response [
84,
85]. These genes include those involved in angiogenesis, glycolysis, cell survival, and apoptosis [
86,
87].
The effect of HIF-2α on insulin secretion in β-cells of mice has been investigated, revealing that metabolic stress induces the activation of HIF-2α, which protects against mitochondrial damage caused by reactive oxygen species (ROS) [
88]. It has also been proposed that, in obesity, metabolic dysregulation activates HIF-1α in adipose tissue macrophages, promoting chronic inflammation and insulin resistance. In obese mice, an increase in HIF-1α, IL-1β, and glycolytic genes was observed. At the same time, the deletion of HIF-1α reduced macrophage accumulation and IL-1β production, highlighting its role in regulating metabolic stress and inflammation in obesity [
89].
This review hypothesizes that chronic exposure to an HFD and PM2.5 promotes a chronically oxidative cellular environment. This condition dysregulates the transcription of genes related to small molecule transport, PPAR and HIF-1 signaling pathways, cytokine–cytokine receptor interactions, and adipogenesis pathways through oxidative modification of transcription factors and DNA methylation enzymes. This study aims to perform a systematic review and a meta-analysis to provide a comprehensive overview of the molecular mechanisms involved in metabolically abnormal obesity induced by HFD and PM2.5 exposure. This study establishes a solid foundation for future research and therapeutic strategies in this field.
4. Discussion
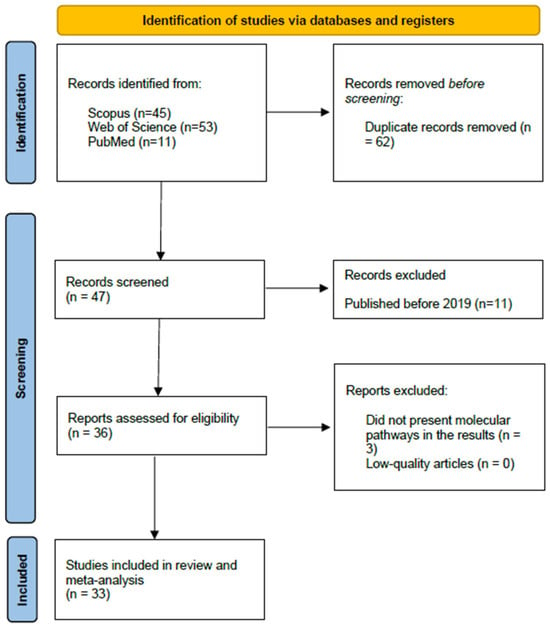
The present systematic review and meta-analysis aimed to form a comprehensive overview of the molecular mechanisms underlying metabolically abnormal obesity induced by an HFD and exposure to PM
2.5. Thirty-three original articles of moderate to high quality, published in journals indexed on Web of Science, Scopus, and PubMed, were analyzed to test the hypothesis that chronic exposure to an HFD and PM
2.5 promotes a chronically oxidative cellular environment, which dysregulates the transcription of genes related to small molecule transport, PPAR and HIF-1 signaling pathways, cytokine–cytokine receptor interaction, and adipogenesis gene pathways through oxidative modification of the transcription factors and enzymes involved in DNA methylation. Our results indicate that combining an HFD and prolonged exposure to PM
2.5 produces a more significant increase in body weight than individual exposure to PM
2.5 or HFD. In contrast, Goettems-Fiorin et al. [
143] observed an increase in weight in murine exposed to HFD and PM
2.5. Still, they did not find statistically significant differences between the control group and those exposed individually or combined to both factors.
Similarly, the review by Guardia and Wang [
144] reports that, in animals exposed to PM
2.5, WAT hypertrophy occurred independently of changes in energy intake. However, this review also mentions that mice exposed to PM
2.5 in utero show microglial activation, increased anxiety, and higher body weight in adulthood compared to the control group, suggesting that prolonged exposure to PM
2.5 could remodel the circuits that regulate the feeding behavior and energy balance. The inconsistency between these results could be due to the high heterogeneity observed in our meta-analysis, both globally and in subgroups, probably related to phenotypic differences in the size of the murine species studied and variations in the design and scope of the investigations.
Based on the oxidative stress biomarkers analyzed, only SOD showed statistically significant results, although with high heterogeneity. SOD is an essential antioxidant enzyme that protects cells from oxidative damage by catalyzing the conversion of superoxide radicals to oxygen and hydrogen peroxide [
145,
146]. An increase in SOD levels usually reflects an adaptive response of the organism to an increase in oxidative stress [
147,
148].
The analysis of the data shows that the combined exposure to HFD and PM
2.5 caused a more notable increase in SOD levels compared to the individual exposures, which recorded similar increases between them. This observation suggests that simultaneous exposure to both factors enhances oxidative damage to a greater extent than exposure to each separately, consistent with our hypothesis that chronic exposure to HFD and PM
2.5 promotes a chronically oxidative cellular environment. The elevation of SOD in this context can be interpreted as an indicator of the organism’s adaptive response to a state of exacerbated oxidative stress. This result coincides with a recent review on the interaction of environmental factors in the metabolic processes of metastasis [
149], suggesting that the combination of HFD and PM
2.5 not only alters the antioxidant response but also contributes to greater cellular vulnerability to oxidative damage. The high variability across the studies analyzed may stem from differences in exposure doses and application frequency, underscoring the need for standardized protocols to accurately assess the effects of these exposures in the context of oxidative stress.
Among the metabolic biomarkers associated with increased body weight, individual exposure to HFD and PM
2.5 was observed to cause significant increases in four parameters: total cholesterol, HDL, insulin, and glucose, with no or low heterogeneity. These results could suggest a mechanistic interaction [
150] between both factors, consistent with our previous study [
20]. On the other hand, combined exposure to HFD and PM
2.5 also led to significant increases in HDL and insulin, with no or low heterogeneity. This finding is relevant since it suggests a biological interaction [
150], indicating a possible synergy in its metabolic impact. Our results align with other recent reviews [
144,
151]. The consistent response in HDL and insulin, even under simultaneous exposure to both factors, underscores the importance of jointly evaluating these exposures when assessing the metabolic risk.
When the transcripts were examined with the biological pathway enrichment analysis, we found that only clusters of three or four genes showed statistically significant results for each molecular pathway in BAT, WAT, heart, and liver tissue. This result supports our hypothesis that chronic exposure to HFD and PM2.5 dysregulates the transcription of genes related to various metabolic pathways. Identifying specific gene clusters with statistical significance suggests that exposure to these environmental factors has a selective impact on regulating particular biological pathways, which could be fundamental to understanding how the interaction between HFD and PM2.5 alters cellular function and contributes to metabolic alterations.
In BAT, PM
2.5 exposure dysregulated
Cebpa,
Pparα,
Serpine1, and
Ucp1 transcripts, affecting genes related to adipogenesis, which is consistent with our previous findings [
20]. On the other hand, HFD altered the regulation of
Tnf,
Lepr, and
Pparα, impacting the adipocytokine signaling pathway, which coincides with the reports of Dogan and Brockmann [
152], who reported that
Pparα, along with other downregulated genes, is involved in inflammatory pathways, particularly in the adipocytokine signaling pathway and in the complement and coagulation cascades in epididymal adipose tissue. These results partially support our hypothesis that chronic exposure to HFD and PM
2.5 deregulates the transcription of genes related to specific biological pathways. Although no evidence was found for some of the hypothesized pathways, such as small-molecule transport and HIF-1 signaling, identifying pathways related to adipogenesis and cytokine regulation is relevant, suggesting that HFD and PM
2.5 interact by affecting complementary pathways [
150]. While HFD promotes a pro-inflammatory environment through the adipocytokine signaling pathway, exposure to PM
2.5 interferes with the ability of BAT to carry out adipogenesis and maintain thermogenesis, exacerbating metabolic dysfunction in this tissue.
In WAT, HFD and PM
2.5 exposure affected the protein metabolism pathway, downregulating
Apoa1,
Apoa5, and
Ghrl transcripts, suggesting an impact on lipid metabolism. However, unlike our initial hypothesis, no significant alterations were observed in the inferred biological pathways. This finding differs from Guerra-Cantera et al. [
153], who observed more significant alterations in this pathway after a low-fat diet. Likewise, minimal changes were reported in the same pathway [
154]. These discrepancies could be due to differences in the time of exposure to HFD and the tissues analyzed since neither study focused on WAT. The concurrent alteration of this pathway by both exposures suggests a mechanistic interaction [
150], possibly amplifying the negative impact on WAT, which could compromise its metabolic and regulatory function.
Individual and combined exposure to HFD and PM
2.5 in liver tissue affects the same pathways. The AMPK signaling pathway showed deregulation of
Fasn,
Scd1, and
Sirt1 transcripts, consistent with other authors [
155,
156,
157] who independently observed similar effects in murine models exposed to HFD or PM
2.5. The affectation of these pathways suggests a possible interaction [
150] between HFD and PM
2.5, intensifying transcriptomic alterations in the liver and potentially aggravating metabolic dysfunctions.
The non-alcoholic fatty liver disease showed a transcriptional alteration in the
Fas,
Pparα, and
Tnf genes, consistent with literature where similar changes induced by HDF were observed [
158,
159]. In addition, a review reports alterations in these transcripts after exposure to PM
2.5 [
160]. The concurrent alteration of these genes is a good proxy of the interaction [
150] between HFD and PM
2.5, which could synergistically affect transcriptional dysregulation, favoring the development, progression, and complication of non-alcoholic fatty liver disease.
In the liver, the PPAR signaling pathway showed deregulation in Acox1, Pparα, and Scd1 transcripts after exposure to HFD, in agreement with Tu et al. [
161]. Consistent with our initial hypothesis, the transcription of
Acox1,
Acs14,
Pparα, and
Scd1 was altered by PM
2.5 [
162,
163]. The identified pooled effect possibly indicates a mechanistic and biological interaction [
150], which enhances the PPAR signaling pathway’s impact and aggravates liver dysfunctions associated with obesity and exposure to PM
2.5.
In cardiac tissue, exposure to HFD combined with PM
2.5 activates pathways related to cellular responses to stress, cellular responses to stimuli, and cellular response to chemical stress, with a downregulation of
Apoa1,
Apoa5, and
Ghrl transcripts, which does not agree with our initial hypothesis. Similar alterations in pulmonary endothelial cells exposed to PM
2.5 and effects in adipocytes after HFD were described in Almeida-Silva et al. [
164] and Jarc and Petan [
165], respectively.
A HFD induces the accumulation of lipid droplets in myocytes, favoring the development of heart disease [
166,
167]. In this context, lipid droplets could modulate the cellular stress response, integrating inflammatory and metabolic processes that affect immune cells and various tissues [
165]. This enhances biological interactions that amplify cellular and metabolic stress, exacerbating dysfunction in cardiac tissue and potentially contributing to the development of heart disease.
A limitation of the performed meta-analysis is the moderate to high heterogeneity observed in some studies, reflected in the I2 index values. Although subgroup analyses were applied to address these differences, variability in biological models, the tissues analyzed, and measurement methods may have contributed to this heterogeneity. While this diversity in experimental conditions can enrich our understanding of the effects of HFD and PM2.5 in different contexts, it also somewhat restricts the ability to generalize the findings to other settings. However, the statistical approaches used to handle heterogeneity allow conclusions to be robust within the limits of the included studies.