1. Introduction
While various diagnostic criteria, such as the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD), have been effective in categorizing TMDs, the relationship between dental occlusion and TMDs remains debated. Some studies have suggested that specific skeletal malocclusions, particularly those related to sagittal and vertical discrepancies, could predispose patients to TMDs. Lateral cephalograms have long been used to examine these craniofacial characteristics, but more recent advances in low-dose cone-beam computed tomography (CBCT) offer a detailed assessment of the TMJ and surrounding structures.
This study identify the morphological profiles and skeletal malocclusions with the highest impact on TMD developments through cephalometric analysis derived from CBCT images. By focusing on cephalometric variables and condylar positioning, this research seeks to provide a deeper understanding of how craniofacial morphology influences the development of TMDs and to highlight potential pathways for more personalized treatment approaches.
2. Temporo-Mandibular Disorders (TMDs)
Temporomandibular disorders (TMDs) are a significant health concern, affecting approximately 5% to 12% of the population. TMDs are the second most prevalent musculoskeletal condition, trailing only chronic back pain, and can result in pain and disability.
TMD-related to pain can impact daily activities, psychosocial functioning, and overall quality of life. Patients frequently seek dental advice for their condition, particularly when it is accompanied by pain.
This led to the introduction of the Axis II protocol, which is divided into sets of self-report screening and comprehensive tools. The screening tools, consisting of 41 questions, assess pain intensity, pain-related disability, psychological distress, functional limitations of the jaw, and parafunctional behaviors. A pain drawing is used to assess the locations of pain.
The comprehensive tools, consisting of 81 questions, provide a detailed assessment of the functional limitations of the jaw and psychological distress, as well as additional constructs of anxiety and the presence of comorbid pain conditions.
2.1. Classification
Group 1: Muscular disorders (most prevalent in the population)
Group 2: Disk displacements
Disk displacement with reduction (reduction refers to the recapture of the disk);
Disk displacement without reduction with limited opening;
Disk displacement without reduction without limited opening.
Group 3: Inflammatory and noninflammatory diseases
In 1994, A. Modesti proposed a more clinical classification that would guide the practitioner in choosing therapy depending on whether it was of muscular or joint origin.
Type I: Muscular syndrome;
Type II: Compressive syndrome with mild initial clicking;
Type III: Compressive syndrome with pronounced clicking;
Type IV: Blockage;
Type V: Dislocation.
2.2. Skeletal Malocclusion and TMDs
Skeletal Class II and III malocclusions can have varying characteristics and can be multifactorial, resulting from both environmental and genetic factors. Class II skeletal malocclusion can be characterized by a hypomandibular condition or lack of breastfeeding; spoiled habits such as prolonged use of a pacifier, bottle, and finger sucking (these factors could lead to the development of such skeletal malocclusion if the spoiled habit is not corrected); or genetics. Another component can be a repositioned mandible, always influenced by such spoiled habits. Conversely, there can be an excessive advancement of the maxilla.
In conclusion, Class III skeletal malocclusion involves a wide range of variables and dental and skeletal characteristics that need to be well diagnosed and distinguished in order to carry out correct therapy. This highlights the importance of a comprehensive and detailed examination for each individual patient. Few studies have investigated the structural dentofacial and orthodontic relationships related to temporomandibular joint (TMJ) disorders.
A study, led by Chung-Ju Hwang and team, centered on the lateral cephalometric features in patients with malocclusion who exhibited symptoms related to temporomandibular joint disorders.
Moreover, Chung-Ju Hwang and his team suggested a distinct classification system for TMJ disorders, incorporating significant and clinically pertinent characteristics.
3. Materials and Methods
3.1. Sample and Study Model
Our study was retrospective, as it began with individuals who had already developed the event of interest.
It examined the exposure to potential risk factors, in this case, the onset of TMDs related to malocclusions.
The study was carried out in the orthognathodontics department of Gabriele D’Annunzio University in Chieti.
A group of 67 patients (comprising both males and females) were examined during the peak period of first visits, which at our university was the spring period from March to June.
The criteria for inclusion in the study were as follows: (a) patients being diagnosed with TMDs for the first time. Patients with a first-time diagnosis were included to study the initial stages of TMDs without the influence of prior treatments or interventions that could skew the morphological assessment; (b) patients aged 18 and above (19 y.o. to 70 y.o.). This criterion ensured that the sample included only adult patients whose craniofacial development was complete. This eliminated any variability that could have arisen from ongoing skeletal growth in younger individuals; (c) patients with accessible medical records, wide-field-of-view cone-beam low dosage, and photographs. These records and imaging techniques were essential for conducting a detailed and accurate analysis of the patients’ craniofacial structures and TMJ morphology. CBCT, in particular, allows for precise cephalometric analysis, which is critical for identifying morphological patterns associated with TMDs.
The criteria for exclusion from the study were: (a) patients with a history of tumors, trauma, surgical interventions in the jaw or facial area These factors could introduce significant variability in craniofacial morphology and TMJ function, making it difficult to attribute observed TMD characteristics to skeletal malocclusions alone. By excluding such cases, the study aimed to isolate the role of dental and skeletal malocclusions in the development of TMDs; (b) presence of fractures and other craniofacial anomalies. These conditions could alter the morphology of the TMJ and surrounding structures, confounding the results. Excluding patients with these conditions ensured a more homogeneous sample, focusing on those whose TMDs may be related to skeletal discrepancies rather than other complicating factors; (c) degenerative disease that implies changes in the bones, ligaments, and muscles.
This selection process ensured that the sample was both representative of typical TMD patients and sufficiently homogeneous to allow for meaningful comparisons and conclusions regarding the relationship between craniofacial morphology and TMDs.
3.2. Cone-Beam and Low-Dose Protocol
3.3. Extraction Data
For the study, telecrania of 67 patients (44 female and 23 male) who had undergone low-dose cone-beam computed tomography (CBCT) in the orthodontics department of Chieti during their initial visit were selected. Each patient’s CBCT was performed with the head oriented according to the natural head position (NHP). The patient was seated with their back as perpendicular to the floor as possible. The head was stabilized using ear rods placed in the external auditory meatus. The patient was asked to look into a mirror 1.5 m in front of them to achieve the NHP and to keep their teeth in contact.
The cranial image was then oriented according to the NHP in three perpendicular spatial planes:
The transverse plane coincided with the Frankfurt horizontal plane (FH), passing through two points: Orbitale (Or) and Porion (Po);
The sagittal plane coincided with the midsagittal plane (MSP), perpendicular to the FH plane and passing through two points: Crista Galli (Cg) and Basion (Ba);
The coronal plane coincided with the anteroposterior plane (PO), perpendicular to both the FH and MSP planes, passing through the right and left portions.
Following head orientation, various 2D virtual radiographs were extracted, including the lateral cephalogram, from which we derived the cephalometric data analysis.
4. Analysis of the Morphological Profiles of Patients with TMDs Through Data from Telecrania and Condylar Sections
Our study also considered gender as a variable, as previous studies have done.
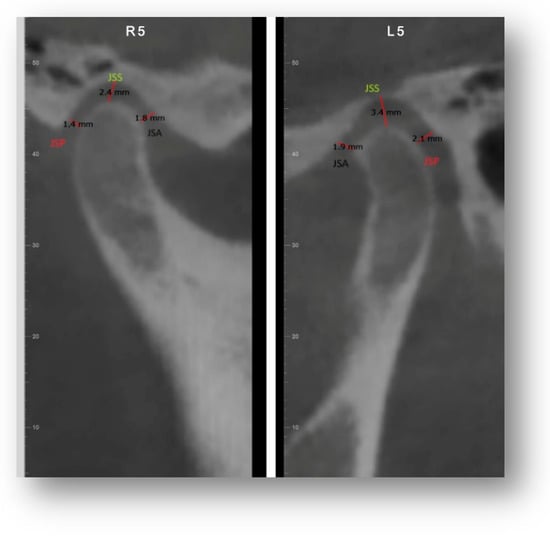
Subsequently, the morphology and position of the condyle of all patients were investigated, taking into account the divergence, thanks to the 3D and 2D sections obtained through the Dolphin software 11.95 from the low-dose cone beam with a wide FOV, which allowed measurements and investigation of anatomical structures at 360°.
Linear Ratio (LR) = (P − A)/(P + A) × 100
where P is the closest posterior measurement and A is the closest anterior measurement.
If LR < −12—posterior position;
If −12 < LR < 12—concentric position;
A vertical distance of 1–4 mm was considered normal; 4 mm: condyle positioned inferiorly; <1 mm: condyle positioned superiorly.
A value of 0 mm was indicated as bone contact.
5. Results
5.1. Cephalometric Data by Sex
The study analyzed cephalometric data from 67 patients (44 females and 23 males) diagnosed with temporomandibular disorders (TMDs). The key findings are summarized below, with visual aids provided to clarify the differences between groups.
Male patients:
Sagittal Profile: Of male patients, 56% exhibited a Class II skeletal profile due to mandibular retrognathia, while 17% showed a Class III profile and 27% had a Class I profile.
Vertical Profile: Of males, 73% were brachyfacial with a hypodivergent pattern, while 20% were normodivergent and 8% were dolichofacial.
Dental Relationships: Increased overjet and a tendency towards deep bite were observed; 23% of male patients presented with a deep bite.
Female Patients:
Sagittal Profile: 79% of females presented with a Class II skeletal profile characterized by mandibular retrognathia, 16% had a Class I profile, and only 8% exhibited a Class III profile.
Vertical Profile: 47% of female patients were hypodivergent, 43% were mesofacial, and 10% were dolichofacial.
Dental Relationships: 48% of females with a Class II profile had an increased overjet, while 17% presented with a deep bite.
5.2. Condyle–Fossa Relationships
The analysis of the condyle position in relation to the glenoid fossa revealed significant differences between sexes and skeletal classes:
5.3. Comparison of Cephalometric Variables
This scheme helps to easily visualize the differences in cephalometric variables between the two groups, clearly illustrating how males and females differed in terms of angles and skeletal measurement.
For example:
FMA Angle: Males with a hypodivergent profile had a lower FMA angle (19°) compared with the normal value of 25°, while females had a slightly higher average (27.58°).
Mandibular Length: Female patients exhibited a shorter mandibular length (70 mm) than males (65.41 mm), which may have contributed to the higher prevalence of Class II profiles among females.
5.4. Gender Differences in TMD Profiles
There was a notable gender difference in the presentation of TMD symptoms, with females more frequently exhibiting Class II profiles and showing a tendency towards mandibular retrognathia.
This pie chart shows the percentage distribution of Class I, II, and III profiles by sex, highlighting the prevalence of Class II in females.
Summary of Findings
A higher prevalence of Class II skeletal profiles was observed in both male (56%) and female (79%) patients with TMDs, although females were more likely to exhibit retrognathia.
Males exhibited a stronger tendency towards a hypodivergent, brachyfacial profile, while females showed a broader range of vertical facial patterns.
6. Discussion
The temporomandibular joint (TMJ) is one of the most sophisticated anatomical elements in the human body, playing a significant role in dental practice.
Consequently, during diagnosis and treatment, physicians should pay particular attention to the position and shape of the mandibular condyle and the patient’s skeletal morphology.
Specific facial structures, such as hyperdivergence or skeletal Class II and III malocclusions, could play a role in the emergence of temporomandibular disorders and their associated symptoms.
6.1. Gender Differences in Skeletal and Morphological Profiles
6.2. Implications of Gender Differences for Diagnosis and Treatment
6.2.1. Diagnostic Implications
The gender differences observed in skeletal profiles have important diagnostic implications. Since females are more likely to exhibit Class II malocclusions and mandibular retrognathia, clinicians must be vigilant in assessing these traits during the diagnosis of TMDs in women. Additionally, hormonal fluctuations, which are more prevalent in females, may exacerbate symptoms and lead to more frequent consultations. This highlights the need for a thorough clinical history, including hormonal influences, to better understand the progression of TMDs in female patients.
For male patients, who are more likely to present with brachyfacial hypodivergent patterns, the emphasis may need to shift towards identifying skeletal discrepancies that could lead to joint compression. Hypodivergent patterns are associated with greater joint compression, which may increase the risk of muscle hypertonia and related pain. This suggests that different cephalometric features, such as mandibular length and FMA angle, should be prioritized when diagnosing TMDs in males.
6.2.2. Treatment Implications
The differences in skeletal morphology between males and females also have significant implications for treatment. In females, the prevalence of mandibular retrognathia (Class II) suggests that treatments aimed at correcting sagittal discrepancies, such as orthodontic appliances or orthognathic surgery, may be particularly effective. Additionally, since women are more likely to experience pain exacerbated by hormonal factors, it may be beneficial to integrate multidisciplinary approaches that include pain management strategies tailored to hormonal cycles.
For males, treatments may need to focus more on managing hypodivergent patterns, which are linked to increased joint compression. Orthopedic interventions that address joint loading and muscular tension could be essential in preventing further degeneration of the temporomandibular joint. Understanding these morphological differences could also aid in preventing the progression of TMDs by addressing structural issues early in treatment.
6.2.3. Broader Understanding of TMDs
These gender-specific differences in skeletal morphology also contribute to the broader understanding of TMDs. Recognizing that TMDs may manifest differently in males and females allows for more precise categorization of the disorder, which could lead to improved diagnostic criteria and treatment protocols.
As for age, one of the inclusion criteria was being of legal age; the average age of women, 41.5 years, was higher than that of men, 35.8 years. In both cases, it was noted that symptoms tended to manifest more frequently after the age of 35.
The comparisons made between our study and previous research have significant implications for the field of orthodontics and temporomandibular disorder management. The alignment of our findings with established research strengthens the evidence for individualized diagnostic and therapeutic approaches based on skeletal morphology.
From our study, as already highlighted by a study by Bjork, patients, both women and men and regardless of skeletal malocclusion, with hyperdivergent facial models have more advanced and higher condyles than those with normal or low FMA angles. These results could have significant implications for understanding the growth and development of the face.
7. Conclusions
This study provides valuable insights into the relationship between craniofacial morphology and temporomandibular disorders (TMDs), revealing important gender-specific differences. Our findings showed that Class II skeletal malocclusions, particularly mandibular retrognathia, were more prevalent in females with TMDs, while males exhibited a higher incidence of brachyfacial hypodivergent profiles. These morphological differences suggest that distinct diagnostic and treatment strategies may be required for male and female patients.
In summary, based on the information gathered from the literature and our study, it can be stated that:
Class II malocclusion is more frequently associated with muscular disorders. However, there is no definitive link in the scientific literature with specific joint problems such as clicks, joint blockage, or dislocations. Consequently, it appears that Class II malocclusion is related only to muscular problems.
We therefore found that the reduced vertical dimension of the face that hypodivergent patients present leads to greater compression of the joint tissues and a consequent muscle hypertonia that causes painful symptoms in patients.
Furthermore, the position of the condyle in relation to the fossa varies significantly based on skeletal class and divergence patterns, with hypodivergent patients showing greater joint compression. This reinforces the importance of individualized diagnostic protocols that consider both skeletal and functional factors.
Finally, it is important to remember that the studies supporting the link between skeletal malocclusions and temporomandibular disorders are few. Therefore, the available information is still limited and sometimes conflicting.
The significance of this study lies in its contribution to a more nuanced understanding of how craniofacial characteristics influence the development and management of TMDs. By identifying specific skeletal patterns associated with TMDs, clinicians can improve treatment planning, potentially leading to more effective, personalized interventions. Future research should focus on expanding the sample size and exploring the interplay between systemic conditions, such as rheumatoid arthritis, and TMDs to provide further insights into the multifactorial nature of this disorder.
To resolve these discrepancies, specific areas for future research are suggested.
Longitudinal studies: Conduct long-term studies to observe the evolution of skeletal malocclusions and temporomandibular disorders over time.
Biomechanical analysis: Examine how biomechanical forces influence the relationship between skeletal malocclusions and temporomandibular disorders.
Genetics: Investigate the role of genetic factors in the predisposition to skeletal malocclusions and temporomandibular disorders.
Therapeutic interventions: Evaluate the effectiveness of various orthodontic and surgical treatments in improving the symptoms of temporomandibular disorders in patients with skeletal malocclusions.
Comparative studies: Compare groups of patients with and without skeletal malocclusions to identify significant differences in temporomandibular disorders.
However, research, thanks in part to the more detailed images provided by the cone-beam CT scan, is progressing in this field.
8. Limitations of the Study
This study was conducted without considering ‘case–control’ patients as a comparison term. Therefore, the results may be limiting on one hand, though on the other hand, they can serve as a basis for future studies, where this topic can be expanded by including a comparison with a group of patients without TMDs.
Moreover, this type of study is useful for identifying associations between risk factors and the event of interest, but it cannot establish a clear temporal sequence.
Source link
Monica Macrì www.mdpi.com