1. Introduction
As reported, there are some interindividual differences in the effectiveness of platelet-rich plasma (PRP) therapy [
1]. These differences may result from many factors, including growth factors’ concentration [
2], sex [
3], age [
4], and genetic variability [
5]. Transforming growth factor beta 1 gene (
TGFB1) seems to be a suitable candidate for analysis of PRP effectiveness in tendinopathy due to its association with wound healing [
6], tendon development [
7], and pain sensation [
8] and its presence in PRP [
9]. The TGF-β1 exerts pleiotropic action on cells depending on the nature of signaling and cell type, e.g., it induces cytostasis, apoptosis, dormancy, and autophagy [
10]. Although initially thought to stimulate cell proliferation, TGF-β1 is a bifunctional regulator that inhibits or stimulates cell division [
6] and significantly accelerates wound healing [
6,
11,
12]. Expression and activation of this cytokine are induced in response to injury, progressing outward from the site of contusion [
6]. Platelets store large amounts of TGF-β1 that are released at the site of the injury and inflammation to attract monocytes and fibroblasts for local tissue repair [
6,
11]. It has also been shown that TGF-β1 stimulates the expression of extracellular matrix (ECM) proteins, such as fibronectin, collagen types I and III, and vascular endothelial growth factor (VEGF) [
6,
12,
13], as well as inhibits degradation of ECM. The latter is observed due to repression of the metalloproteinases (MMP) expression [
6,
12] and stimulation of tissue inhibitor of metalloproteinases (TIMPs) synthesis [
6]. Furthermore, TGF-β1 stimulates angiogenic properties of endothelial progenitor cells, facilitating blood flow to the damaged site [
8] and plays a pivotal role in fracture healing [
14]. Nevertheless, overexpression of this growth factor may lead to fibrosis, scar formation [
11,
12,
13], and alteration in tissue architecture, which may further affect its physiological function [
15]. Therefore, in the early stage of injury, TGF-β1 can reduce inflammation and accelerate wound healing, although, at the late stage, it may lead to tissue scarring [
16].
The
TGFB1 is expressed in the tendon and likely plays a role in its development [
7]. It has been shown that TGF-β1 inhibits the expression of scleraxis and promotes the expression of tenomodulin [
17]. Scleraxis is expressed at an early stage of tendon development, initiates tendon differentiation, and inhibits the maturation of collagen fibers during tenogenic differentiation, while tenomodulin is a marker of mature tendon cells and accelerates tendon development [
16]. The TGF-β1 also promotes tendon stem cell proliferation and migration, which is beneficial for the treatment of damaged tendons [
18]. Additionally, TGF-β1 stimulates the expression of collagen and can reduce inflammatory response [
12], which can stimulate tendon healing.
The TGF-β1 also appears to be involved in pain perception. This cytokine is an important mediator of nociception and has a protective effect against the development of chronic neuropathic pain by inhibiting neuroimmune responses [
19]. Studies in mice have shown that TGF-β1 secreted from bone marrow stromal cells inhibits neuropathic pain [
20], as well as exhibits antinociceptive properties in a model of lumbar dorsal root ganglia inflammation [
21]. In studies on rats, TGF-β1 was observed to prevent the development of pain and inflammation during intervertebral disc degeneration [
22]. Studies on humans have shown that in patients with osteoporosis, the level of TGF-β1 decreased with increased pain intensity (both in plasma and central cerebral spinal fluid), suggesting that this growth factor might alleviate pain [
8]. However, other studies have shown the opposite results, stating that TGF-β1 has pro-pain properties [
21,
23,
24]. The TGF-β1 contributed to the development of pain sensations in both mouse and rat models of bone cancer [
23] and was involved in hyperalgesia in rats with chronic pancreatitis [
24]. The reasons for these discrepancies are not clear, although they illustrate the vast array of signaling pathways activated by TGF-β1. It is suspected that the effect of TGF-β1 on pain perception depends on the transforming growth factor beta receptor 1 (TGF-βR1) and the activated signaling pathway [
21].
Considering that TGF-β1 exerts pleiotropic effects on cells and tissues, its impact on the effectiveness of tendinopathy treatment with the use of PRP is unknown and, so far, has not been studied. Therefore, in the present study, we analyzed the possible association between four single nucleotide polymorphism (SNPs) of the TGFB1 gene (namely, rs2278422, rs12461895, rs4803455, and rs2241717), with clinical phenotype of lateral elbow tendinopathy (LET), pain perception, and PRP therapy effectiveness of LET treatment.
3. Discussion
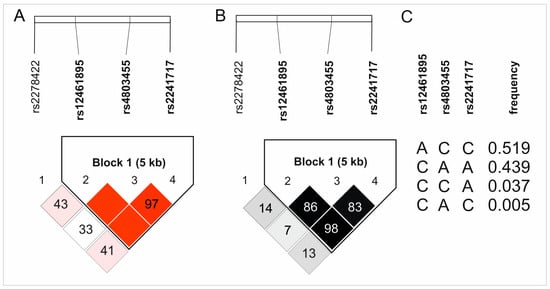
In the present study, it has been demonstrated that analyzed genetic variants of the TGFB1 gene may have an impact on PRP therapy. Better effectiveness of the PRP therapy was observed in rs2278422 CC homozygotes, and this SNP showed no change in pain levels prior to treatment. The contribution of rs12461895, rs4803455, and rs2241717 polymorphisms to the therapy effectiveness is uncertain due to higher values of VAS at day 0 for carriers of the AA, CC, and CC genotypes (rs12461895, rs4803455, rs2241717, respectively). The influence of the analyzed polymorphisms on pain parameters before PRP injection may distort the obtained results. It is worth noting that this most likely results from the involvement of TGF-β1 in pain sensation. The presence of studied SNPs correlated with the results of blood morphological parameters and pain perception. Numerous significant results after applying the Hochberg correction, indicating a clear relationship between the tested SNPs (especially rs2278422) and the effectiveness of PRP treatment, support an association between the analyzed polymorphisms and PRP therapy outcomes.
Rs12461895, rs4803455, and rs2241717 polymorphisms formed a haplotype; hence, the results obtained were similar. Since ΔVAS is the difference between the pain level on day 0 and a specific follow-up point, a higher VAS on day 0 experienced by the AA, CC, and CC homozygotes (rs12461895, rs4803455, and rs2241717, respectively) will modify the ΔVAS value. Interestingly, patients with these genotypes also showed higher ΔVAS values. This means that despite the stronger pain they felt before starting the therapy, they still showed improvement. Whether this improvement is actually greater than in carriers of the other genotypes remains debatable. The influence of these polymorphisms on pain sensation is also visible in other analyses. Patients with these genotypes were characterized by more frequent pain during elbow bending. These results do not seem accidental due to many reports suggesting TGF-β1 role in pain perception. As mentioned, the influence of TGF-β1 on pain may differ, probably dependently on TGF-β1-mediated signaling [
21]; however, studies on human osteoporosis have shown that higher levels of TGF-β1 may alleviate pain [
8]. Of the polymorphisms we analyzed, rs4803455 is the most widely studied. It has been shown that carriers of the A allele had a reduced risk of asthma [
26], carotid plaque formation [
27], breast and endometrial cancer [
28,
29], as well as post-transplant renal dysfunction [
30]. However, there are no reports available in the literature presenting the rs4803455 effect on
TGFB1 expression. In silico analyses showed that CC genotypes of the rs4803455 and rs2241717 polymorphisms are associated with decreased
TGFB1 expression levels in whole blood (
Figure 4). Although these results are not statistically significant, a certain trend can be observed. It appears that genotypes associated with decreased
TGFB1 expression are also associated with elevated levels of pain, which is consistent with the study of Liu et al. [
8] and confirms the analgesic effect of TGF-β1 in human musculoskeletal tissues. Because PRP contains a high concentration of TGF-β1 [
9], it is possible that PRP administration alleviates the pain experienced by patients. This may explain the results obtained in this study.
As previously discussed, we obtained slightly different results for rs2278422 polymorphism compared to other analyzed SNPs. This SNP is located out of the haplotype and did not show any association with pain sensation. We did not observe any differences in either PROM values before PRP injection or pain sensation during elbow bending; however, it showed an association with PRP effectiveness. Patients with the CC genotype showed better therapeutical effectiveness compared to carriers of other genotypes. Previous studies have shown that the CG genotype of this polymorphism is associated with a reduced risk of osteoarthritis [
32], while GG homozygotes had a lower risk of insulin resistance [
33]. No information is available in the literature about the rs2278422 effect on the expression of
TGFB1. In silico analyses demonstrated a trend indicating increased
TGFB1 expression in the CC genotype, but the results are not statistically significant (
Figure 5). Interestingly, the genotype that was associated with a better effect of PRP therapy was associated with raised levels of
TGFB1 expression. Perhaps a reduced expression level of
TGFB1 leads to increased pain, whereas the elevated expression leads to better therapeutic progress due to the involvement of TGF-β1 in the regeneration of the damaged tendon [
17].
Tendinopathy is a series of changes occurring in tendons, which lead to pain and impaired function. In a damaged tendon, collagen fibers are disorganized, and ECM remodeling, proliferation, as well as angiogenesis are dysregulated [
34]. It should be emphasized that many proteins can potentially affect the pathogenesis of tendinopathy. MMPs and their inhibitors have an important role in tissue remodeling [
35], and polymorphisms of the
MMP3 and
TIMP2 genes are associated with the risk of Achilles tendinopathy (AT) [
36]. Moreover, tenocytes and immune cells release pro-inflammatory factors in response to tissue injury, such as tumor necrosis factor (TNF), interleukin 1 beta (IL-1β), interleukin 6 (IL-6), TGF-βs, and platelet-derived growth factors (PDGFs) [
34]. It was shown that polymorphisms of
IL-1β and
IL-6 genes are also associated with AT [
37]. In the same study,
COL5A1 gene SNP association with the risk of Achilles tendinopathy was also shown [
37]. Since tendons are composed of collagen, it seems probable that polymorphisms in the genes encoding these proteins will also influence the pathogenesis of tendinopathy. Interestingly enough, other studies indicate that collagen has a role in pain perception as well [
38]. It is important to note that factors influencing the pathogenesis of tendinopathy may also modify the effectiveness of its treatment and the level of pain. The studies we have conducted so far indicate that polymorphisms of genes encoding cytokines from the PDGF/VEGF superfamily [
39,
40,
41,
42] and PDGF receptors (PDGFR) [
43,
44] are associated with the effectiveness of PRP, while
COL1A1 gene SNPs showed association mainly with pain sensations [
45]. This indicates a wide range of factors potentially modulating the effectiveness of tendinopathy treatment using PRP therapy, which results from the fact that many factors are involved in its pathogenesis. Moreover, the growth factors and their receptors that we have studied previously can interact with each other and with TGF-β1. It has been shown that VEGFA can bind to PDGFR [
46], while PDGFRB interacts with TGF-beta signaling [
47]. This adds an additional layer of complexity to the factors potentially modulating the treatment of tendinopathy and their interactions.
The current work also provides interesting observations of the analyzed TGF-β1 variant’s association with the results of blood morphological parameters. Investigated polymorphisms showed an association, among others, with MPV, PLT, PDW, NEU, EOS, and MONO levels. Those associations may be justified by the participation of TGF-β1 in hematopoiesis. In vitro studies have shown that TGF-β1 inhibits hematopoiesis [
48,
49,
50]; however, the functions of TGF-β1 are largely determined by the environment, cell type, and differentiation level [
51,
52]. In vivo studies of TGF-β1 in a mouse model have shown that loss of this protein leads to a decrease in proteins indispensable for hemopoiesis, which may cause its defects [
49]. Furthermore, TGF-β1 determines hematopoietic stem cell (HSC) fate and maintains the self-renewal ability of HSCs in vivo [
48]. This indicates a significant and not fully understood role of TGF-β1 in the regulation of hematopoiesis.
Rs2278422, rs4803455, and rs2241717 showed an association with platelet parameters, which is particularly important in the context of PRP effectiveness. Although these results were not statistically significant after correction, a certain trend was observed. In the dominant/recessive model, the C allele of the rs2278422 polymorphism, which was associated with a better effect of PRP therapy, was also associated with increased values of MPV. This is consistent with our previous results indicating that larger platelets are more active, which positively translates into PRP activity [
43]. Moreover, the AA genotype of rs2241717 was associated with higher PLT levels and the C allele of rs4803455 with higher PDW (
Table 2). Interestingly, studies indicate that TGF-β1 inhibits megakaryopoiesis [
53,
54,
55,
56]. Since TGF-β1 is produced in large amounts by megakaryocytes and platelets, this growth factor could be considered a possible feedback regulator of megakaryopoiesis [
53,
56]. However, studies in TGF-β1 knockout mice have shown that loss of TGF-β1 function leads to a decrease in the amount of megakaryocyte–erythroid progenitor cells (MEPs) [
49]. There is a lack of information in the literature on the effect of TGF-β1 on platelet parameters; therefore, we do not know how polymorphisms investigated in this study could affect the MPV, PLT, and PDW parameters. Moreover, due to the bifunctional action of TGF-β1 and the above-mentioned studies on TGF-β1-deficient mice, it is difficult to definitively determine how TGF-β1 affects platelet formation.
Moreover, analyzed polymorphisms also showed an association with the results of monocytes, eosinophils, and neutrophils levels. The literature data indicate that TGF-β1 may influence neutrophil signaling and gene expression but not migration [
57], inhibit eosinophils recruitment [
58] and induce their degranulation [
59], as well as promote the maturation and differentiation of monocytic cells [
52]. It was shown that loss of TGF-β1 function also led to a decrease in the number of granulocyte–monocyte progenitor cells (GMPs) [
49], which can affect neutrophil, eosinophil, and monocyte levels. In our study, the AC heterozygotes (additive model) and carriers of the C allele (dominant/recessive model) of rs4803455 had higher levels of NEU, and the AC genotype was associated with the highest level of
TGFB1 expression in in silico analysis. Carriers of these genotypes also had lower EOS percentages (additive model), which may be associated with TGF-β1’s role in eosinophil recruitment inhibition. In the case of monocytes, the C allele of rs224171, which was associated with lower
TGFB1 expression, was also associated with lower levels of MONO (
Table 2,
Supplementary Table S1,
Figure 4). Circumstantial information available in the literature is consistent with our results; however, determining the influence of the studied SNPs on blood morphological parameters requires further studies. Due to the questionable influence of rs4803455 and rs224171 polymorphisms on the effectiveness of PRP therapy, it is also difficult to determine whether these changes in the patients’ blood counts could affect the effectiveness of the treatment.
The main limitations of our study are the relatively small study group and the lack of restrictions on other forms of therapy after PRP injection. The lack of limitations for other forms of therapy results from ethical issues. In our opinion, denying access to other forms of treatment for two years to patients for whom PRP therapy was not effective is unethical. Moreover, to reduce the risk of falsely positive results, we performed both quantitative and qualitative analysis and applied a correction for multiple tests. Nevertheless, confirmation of the obtained results requires more detailed research on a larger study group. In particular, determining the influence of the analyzed SNPs on the TGFB1 expression would enable a better understanding of their exact function.