1. Introduction
Based on Kessler et al. [
1] and according to the “Health at a Glance Europe 2018” report, approximately 84 million people in the EU are affected by mental health problems, with both depression and anxiety disorders being the first and sixth leading causes of disability, respectively [
2]. The “Health at a Glance Europe report 2022” showed that almost one in two young Europeans reported a need for psychosocial support [
3]. In addition to the personal suffering of those affected, mental health problems have a considerable financial impact on society. The total costs of mental illnesses are more than 4% of the GDP of the 27 EU countries and the United Kingdom, or over EUR 600 billion [
3]. Apart from this, the mortality rate for people with mental illness is two to three times higher as compared to the general population [
4,
5], thus shortening life expectancy up to 15 years [
6,
7,
8]. This is partly due to people with affective disorders showing an increased risk of developing a metabolic syndrome [
9] and type 2 diabetes mellitus [
10]. To counteract this development, an active lifestyle and regular physical exercise seem to be effective methods [
11,
12]. Reported benefits of physical activity for people with mental illness are symptom reduction, improved cardiovascular risk profile, and improved physical capacity [
13]. Furthermore, an active lifestyle has been linked to mental health and well-being [
14]. Stanton et al. [
15] highlighted the benefits of physical activity for individuals with mental health problems alongside pharmacological and psychological interventions. However, it has been shown that psychotropic medication (antipsychotics, antidepressants, and mood stabilizers) was associated with an increased risk for several physical diseases [
16], thus highlighting the importance of physical activity and exercise as an effective complement in the treatment of mental diseases.
Several meta-analyses indicate antidepressant effects of physical activity in people with depression [
17,
18,
19,
20]. For this reason, the European Psychiatric Association identified physical activity as an important primary or adjunct strategy in the treatment of depression [
21]. Heissel et al. [
22] confirmed the role of physical exercise for depressive disorder and recommend that exercise should be offered as an evidence-based treatment option, supervised, and offered as a group exercise at moderate aerobic intensity. However, it was also mentioned, critically, that more high-quality trials are needed to determine valid parameters for physical performance, as well as to evaluate programs to motivate patients to maintain their exercise after discharge from a hospital setting [
23].
The level of cardiorespiratory fitness (CRF) is an important measure of physical status and a strong predictor of all-cause mortality [
24]. CRF level is also associated with the risk of common mental health disorders [
25]. With regard to the call for evidence-based exercise treatment, only few data are available on CRF and performance measures related to health-related variables in patients diagnosed with affective disorders. This is somehow surprising, as the evaluation of the current physical performance level of individuals builds up the basis for target-orientated and efficient exercise treatment. Herbsleb et al. [
26] showed that CRF was expected to be significantly lower in patients with major depression (MDD) compared to healthy controls, indicated by lower peak oxygen uptake and peak power output, similar to Gerber et al. [
27], who showed a lower CRF in patients with first or recurrent depression and bipolar disorder type II (currently depressed, based on the International Classification of Diseases, 10th Revision [
28]) compared to healthy controls. Most recently, Kreppke et al. [
29] also showed that among patients with major depressive disorder, those with particularly high self-assessed severity scores showed lower CRF and less favorable perceived fitness compared to healthy controls. It is difficult to state whether a lower CRF is a consequence or the cause of depression, as both factors influence each other in a vicious circle. However, patients with good CRF were shown to have more favorable scores across cardiorespiratory risk markers (e.g., high body fat, hypertension) than counterparts with poor CRF.
Aiming for higher CRF in people with mental illness, exercise interventions were shown to have a moderate effect on increasing CRF to clinically relevant levels among people experiencing depression [
30,
31]. Studies showed that regular exercise increases CRF [
31,
32] and can even lead to a significantly stronger reduction in depressive symptoms compared to usual care without regular exercise [
32]. Additionally, physical fitness was shown to be a stronger predictor for the onset of depressive symptoms compared to being overweight or obese [
33]. CRF, therefore, appears to be a central resource in the prevention and treatment of depressive disorders and other mental illnesses. However, to the authors’ knowledge, there is yet no clear connection between changes in CRF and depression scores [
26]. In addition, there is a well-known relationship between CRF and several chronic diseases, such as cardiovascular or metabolic diseases, which are often combined with depressive disorders [
9,
13].
Although a growing body of literature supports the notion that exercise and physical activity interventions have beneficial effects across several physical and mental-health outcomes [
30,
33,
34], almost no data are available on exercise performance, its changes, and its association with changes in mental health during a standardized psychiatric rehabilitation program of patients with mental disorders. However, this is of great interest, as the necessity of a stay in a psychiatric rehabilitation increased locally by +21.6% compared to 2019 and by +29.1% compared to 2020 [
35], which is also shown in recent European statistics [
36]. These numbers not only represent the increasing need for psychiatric rehabilitation but also reflect the rise in mental health problems in the population. This makes the development of targeted and sustainable measures increasingly important. Therefore, the aim of the study was to investigate exercise performance at the beginning of a rehabilitation program, as well as changes in performance during a 6-week standardized rehabilitation program in a specialized rehabilitation clinic and to relate the changes to clinical outcomes and the severity of depression symptoms. We hypothesize that people with a lower depression score have better physical performance than people with higher depression symptoms, as well as that the standard rehabilitation program will not lead to performance increases. Furthermore, we were exploratively interested whether patients with a psychiatric diagnosis are willing to safely push themselves physically to their personal limit during exercise testing.
4. Discussion
In the present study, we explored cardiorespiratory fitness (CRF) in patients with a primary diagnosis of depression at the beginning and at the end of their 6-week stay in an Austrian rehabilitation center specialized in psychiatric illness and its association with the severity of depression symptoms. Overall, we could show that CRF significantly increased, and depression score and physiological distress significantly decreased, after the end of the stay. Additionally, increased performance was significantly related to improvements in the severity of depression symptoms. Against our two hypotheses, the severity of depression was not related to the performance level at the start of the rehabilitation and performance increased significantly during the rehabilitation program.
Notably, a maximal incremental exercise test to determine CRF was feasible in all participants included in the study, independent of their physical status and the severity of their mental disorder, with 89% of the participants reaching maximal volitional exhaustion according to standard criteria. A similar finding was reported by Boettger et al. [
42], indicating a mean RER of 1.11 following a standardized maximal incremental exercise test on a cycle ergometer in 15 patients with major depressive disorder. This is not limited to depression only but has also been demonstrated in patients with other mental disorders like bipolar disorder [
43] or schizophrenia [
44].
Patients’ performance levels in our study at the start of the rehabilitation were quite heterogenous though, with almost half of the patients performing below and almost half within the age- and gender-predicted norm levels of performance for incremental cycle ergometer exercise [
38]. Only nine patients performed above predicted normative values. Mean VO
2max was comparable to a sample of male and female patients with major depressive disorder [
42]. The depression score of most patients in our study was in a mild to moderate range; five individuals reached values below a clinically relevant score (BDI ≤ 12) and eleven fulfilled the criteria of a major depression (BDI ≥ 29). Our hypothesis that people with a lower level of depression show higher CRF at the beginning of the rehabilitation stay could not be confirmed. This was somehow surprising and unexpected, as some reviews found the severity of depression to be inversely correlated with CRF [
25,
45]. These authors also highlighted CRF as a valid and important parameter for identifying and preventing mental health disorders. A study by Thirlaway et al. [
46] confirmed such an inverse association between CRF and depressive symptoms but only for those who were physically inactive, not for those who were at least moderately active. The authors suggested that not only the level of CRF determines such an inverse relationship with depression but also the current individual activity level. We may therefore suggest that acute effects of physical activity and exercise are the main influence on depressive symptoms, explaining the finding of no relation between CRF and the severity of depression in our results, although we did not obtain home-based activity measures before the rehabilitation stay.
It is important to note that the performance levels of patients (and, of course, in general) were rather different at the start of the rehabilitation, while the exercise program during rehabilitation was the same. To achieve training effects, the intensity of exercise should generally be above a certain individual level. However, the current exercise program lacks individuality, which may lead to patients being either over- or underchallenged in such a standardized program. It is important to mention that, compared to underchallenge, an overchallenged situation presents some more risks and could have negative consequences especially in individuals suffering from a chronic disease [
47]. The relevance of our results is additionally underpinned by scientific results that go beyond the basic correlation between physical activity and mental health [
48], focusing more on the impact of the intensity of physical activity and exercise on mental health. A recent review on the effects of exercise on depression [
49] showed a clear dose–response relationship for exercise intensity across exercise modalities. Some modalities (yoga, walking, or strength training, among others) showed higher effects in men or women or depending on age, but benefits tended to be proportional to the intensity only. This is in line with other studies, where the highest effects have been observed at moderate and high intensity, but not at low intensity, of physical activity [
50,
51,
52]. In order to utilize the optimum effect of exercise and training in a rehabilitation setting, our data support the need to determine the physical performance of each patient at the beginning of their program to be able to adjust the intensity of the training individually with respect to a personalized medicine approach [
53].
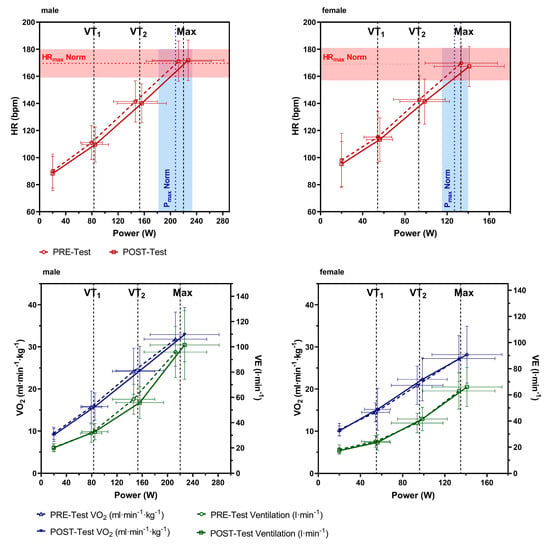
Although there was no individualized exercise program in our study and the time span of 6 weeks was relatively short, with low to moderate intensity on average, performance in maximal incremental cycle ergometer exercise was significantly increased after the stay. In greater detail, performance increased in the majority (66%) of the patients, stayed the same in 30%, and decreased in 4%. Also, performance at sub-maximal values increased and the mean heart rate curve (
Figure 2) showed a clear right shift from pre- to post-test, confirming a performance increase due to training adaptions, thus excluding motivational factors or day-to-day variability. However, increases in VO
2max were lower than the suggested minimal clinically important difference (MCID) of at least 3.5 mL·min
−1·kg
−1 [
54]. The performance increase was similar at VT
1 and VT
2 and increased across the entire performance spectrum. This was to be expected, since, as already mentioned, there were no specific individual training sessions focusing on specific adaptations, like an increase in the aerobic or anaerobic performance. This could be of interest, as Chu et al. [
55] showed that higher-intensity (65–75% MaxVO
2reserve) compared to lower-intensity (40–55% MaxVO
2reserve) exercise training once a week for 30–40 min for 10 weeks led to a comparable decrease in the BDI score, and the higher-intensity aerobic exercise program appeared to be more effective in reducing symptoms of depression. The increase in performance in our study was likely caused by the high total amount of physical activity per day as indicated by the high number of total steps per day. Completing the daily therapy plan alone involves a high level of activity, as the different therapies take place in different rooms and on different floors. Patients reported that they moved significantly more every day than in their daily routine. In addition, they reported to be much more active in their free time, as the rehabilitation center is located in the countryside and offers patients the opportunity to go for a walk outside.
Additionally, it was found that the pre-to-post-rehabilitation changes in maximal performance were significant but independent of the individual performance level at the start of rehabilitation. However, the increase in performance was greater in the 25% lowest-performing, as well as the highest-performing, patients. This can be explained by the fact that less-fit individuals have a higher potential to increase performance compared to individuals with a higher fitness level or with a larger number of exercise or training hours completed (ceiling effects). Hence, although the fittest individuals should increase less, they increased more as compared to the mean. This could be explained by the fact that the physically fittest 25% of the patients were still not well-trained individuals and still had a high potential for development; in addition, this group might have a higher motivation and therefore work harder during the sessions as compared to the others. It is important to note that 30% of patients did not improve their physical performance. An individualized training program might have led to a lower percentage of non-responders to the standardized exercise program, although intensity was not monitored during the exercise sessions.
VO
2max also significantly increased, by around 1.35 mL·min
−1·kg
−1 (3.29%) at constant body weight, which is more than double the growth shown after a supervised aerobic exercise intervention of 90 min of training per week [
31]. Looking at the VO
2peak trainability of structured interval and moderate continuous training, a multi-center comparison from Wiliams et al. [
54] presented an increase of 2.4 mL·min
−1·kg
−1 for continuous training and of 3.3 mL·min
−1·kg
−1 for interval training when results were, among others, adjusted for sex, age, and number of training sessions. Both individualization and a more structured training concept offer potential for an even greater increase in VO
2max within the stay. Since the VO
2max increase within the rehabilitation was markedly lower than the MCID, which is associated with a 10–25% decreased risk of all-cause mortality [
56], adaptation of the exercise concept could be of interest.
Regarding changes in mental health, our data show overall decreased depression symptoms, from moderate depression at the beginning to minimal depression symptoms at the end of the rehabilitation stay. A comparable finding could be shown for BSI, which also indicated a significant reduction in patients’ subjective impairments due to physical and psychological symptoms. It has already been shown that exercise significantly increased cardiorespiratory fitness in people with depression [
30] and positively influenced the severity [
32,
55]. Stubbs et al. [
30] also showed a statistical trend for higher baseline depressive symptoms to predict smaller increases in CRF following 12-week-long, planned, structured, and repetitive exercise interventions. This is contrary to our findings, where the increase in performance was not related to the severity of depression symptoms at the start of the rehabilitation program. However, an increase in performance was shown to be not necessarily accompanied by a reduction in the severity of depression [
31]. It may be suggested that the effects of exercise are not only due to the activity itself but are also influenced by other factors that go hand in hand with it. Noetel et al. [
49] already hypothesized that a combination of social interaction, mindfulness or experiential acceptance, increased self-efficacy, immersion in green spaces, neurobiological mechanisms, and acute positive affects due to exercise combine to generate outcomes. Many types of exercise cover some of these factors but no single one covers all mechanisms.
However, in our study, linear regression analysis showed that changes in P
max could predict significant changes in BDI but not for BSI scores. Looking at the relative changes, we found an improvement of approximately 53% in the BDI but only of 16% in the BSI score, causing less statistical power possibly explaining the effects. For BDI, each watt of improvement in P
max was related to an improvement in the BDI score. However, the linear regression coefficient was small, and the model only explained 10% of the variance. Interestingly, performance changes at VT
1 and VT
2 were more strongly related to changes in BDI score compared to P
max. Therefore, these values seemed to be a better predictor of mental health, with the advantage that no maximal cardiorespiratory test must be carried out. A study by Blumenthal et al. [
32] already showed significantly stronger improvements in BDI score when patients engaged regularly in physical exercise (90 min/week) for three months in addition to their usual treatment relative to not exercising. Furthermore, patients with a BDI score ≥ 14 were shown to benefit even more from additional regular exercise as compared to individuals below this score. However, this study did not investigate the relation between changes in physical performance and changes in BDI. Regarding this relation, there are also results complementary to ours showing a substantial increase in performance (15% in P
max/kg, 19% in VO
2max/kg) and a decrease in the Hamilton-17 depression scale by 2–3 points, independent of the increase in performance [
31]. At present, no clear causality can be established between physical performance changes and the severity of depression symptoms. In general, performance improves as a result of regular exercise. As already mentioned, it is unclear to what extent performance-related physiological adaptations or social and environmental effects of exercise influence changes in mental health. Also, an improved mental health status following six weeks of rehabilitation is a sum effect of all therapies. Each specific effect of each specific therapy cannot be determined in such a real-world approach. It should be emphasized, however, that performance is a resource which can be developed to a considerable degree by well-known methods. This offers great potential to improve the mental health status of individuals with depressive symptoms and even greater potential for reducing comorbidities [
24,
36].
In addition to general effects, several studies also showed biological effects of exercise training related to the disease. Recently, Gujral et al. [
57] showed that acutely depressed adults presented regional gray-matter abnormalities, as well as abnormalities in other brain regions. Exercise was shown to positively influence these structures, e.g., hippocampal volume, and the evidence was described as promising. Although these authors reported inconsistencies between types and duration of exercise, precluding a clear understanding of the underlying effects, they concluded that moderate-intensity aerobic exercise, as a non-pharmacological strategy, improves hippocampal volume, supporting the assumption of intensity as an important variable. Additionally, evidence was reported for a positive relationship between CRF, physical activity, and prefrontal cortex volume. Similar effects were prescribed for striatum and white matter integrity by these authors [
57]. In addition to the prescribed effects of exercise on brain structures, it was recently shown by Ross et al. [
58] that acute bouts of exercise are able to modulate circulating levels of serotonin and norepinephrine, brain-derived neurotrophic factor, and a variety of immuno-inflammatory mechanisms in clinical cohorts with depression. However, these authors argue that chronic exercise training has not been demonstrated to consistently modulate such mechanisms, and evidence linking these putative mechanisms and reductions in depression is lacking. They also highlighted that the complexity of the biological underpinnings of depression coupled with the complicated molecular cascade induced by exercise are significant barriers to understanding the effects of exercise on depression. Despite these limitations, clinical evidence uniformly argues for the application of exercise to treat depression [
58].
Nevertheless, more studies focusing on exercise effects are of potential interest. In particular, randomized controlled trials investigating these effects in a rehabilitation setting, as well as in patient care, appear mandatory.
Limitations
Some limitations of the study need to be mentioned. Our results are limited to individuals in a rehabilitation setting and cannot be transferred to those with an acute status of affective disorders; those with neurotic, stress, and somatoform disorders; or individuals with overly strong depressive symptoms. Furthermore, patients were pre-selected before they were included in the study, at the start of rehabilitation, in order to minimize cardiac risk. Therefore, individuals with cardiovascular or other diseases are not represented in the actual analysis. However, although participants were pre-selected, there was high heterogeneity in exercise performance, as well as in the severity of depression symptoms. Inclusion of patients with comorbidities will be important for future studies and may allow more general conclusions. We also did not analyze the effects of medication in combination with the rehabilitation program on the improvement in depression. However, as medication did not change, we suggest that the improvements were due to the program (exercise and other therapies) but cannot exclude interactions between those factors. Regarding the evaluation of mental health, the self-assessment tools used to evaluate the severity of depression (BDI and BSI) are partly a limit compared to a more objective assessment by a physician. Furthermore, there was no control of the intensity of the standardized exercise program. Monitoring the intensity of the sessions would have allowed us to assign performance effects, as well as changes in mental health status, to specific exercise and training stimuli. Future studies should focus on this in order to determine more precisely the cause of the physical and mental adaptations during rehabilitation. It should also be mentioned that in the present study we did not record the status of physical activity prior to the rehabilitation stay, which would have provided additional information about the relationship between CRF and the severity of depressive symptoms. Furthermore, a control group is missing, meaning patients who are registered for a rehabilitation stay but are on a waiting list. This was not possible due to the current data protection regulations.