1. Introduction
Antimicrobial medications are pharmacological agents implemented in the treatment of infections induced by microorganisms, which encompass bacteria, viruses, fungi, and parasites. These agents operate through mechanisms that either eliminate pathogens or suppress their proliferation, thus facilitating the resolution of infections and mitigate their transmission. Their development and application have significantly diminished the morbidity and mortality linked to infectious diseases [
1,
2,
3,
4].
During the previous decade, over-the-counter systemic antibiotic prescriptions from community pharmacists have risen considerably internationally [
5,
6]. The antimicrobial stewardship protocols are recommended for proper antibiotic prescribing to reduce antimicrobial resistance in Jordan [
7]. Consequently, ensuring patient access to antibiotics through pharmacies poses a significant challenge for international organizations striving to combat the widespread emergence of antibiotic-resistant mutations, which represent a serious global health threat [
8].
The prescription of antimicrobial medications constitutes a fundamental component of medical practice, necessitating meticulous consideration and disciplinary knowledge. The process entails a selection of an appropriate antimicrobial agent contingent upon the specific type of infection, the suspected or confirmed causative microorganism, and the individual characteristics of the patient, including age, renal function, and allergy history. Accurate diagnosis and susceptibility testing are essential to confirm the efficacy of the selected antimicrobial agent against the pathogen [
9]. Furthermore, it is essential to carefully ascertain the dosage, route of administration, and duration of treatment to optimize efficacy while concurrently reducing the likelihood of adverse effects and the emergence of resistance. Healthcare providers are required to inform patients regarding the significance of adhering to the prescribed treatment plan, the possible adverse effects, and the risks associated with misuse, including the omission of doses or the utilization of surplus antibiotics. Adherence to appropriate antimicrobial guidelines is crucial for maintaining the efficacy of these essential medications, mitigating the prevalence of antimicrobial resistance, and guaranteeing optimal patient outcomes [
10].
The widespread administration of antibiotics in the absence of a prescription or appropriate medical oversight may facilitate the emergence of multidrug-resistant pathogens. Antimicrobial agents serve as essential tools in the management and prophylaxis of infectious diseases. Their appropriate utilization, in conjunction with ongoing research and development, is essential to maintain their efficacy and tackle the growing issue of antimicrobial resistance.
As healthcare professionals, pharmacists in Jordan and other surrounding countries play an integral role in antibiotic over-the-counter prescriptions [
11,
12,
13]. This attitude exaggerates the resistance against antibiotics globally, especially in the case of an inappropriate need for antibiotics, self-medication, and consumption behaviors [
14]. This impactful problem fires the alarm to face another suspected multidrug-resistant bacterial pandemic, especially after the COVID-19 pandemic [
15,
16]. In this study, we investigated over-the-counter prescriptions of antibiotics in Jordan, in addition to exploring pharmacists’ antibiotic selections according to their practices. Here, we evaluate the source of information and confidence of prescribing antimicrobials, the type of prescribed antimicrobials, the occurrences of requesting non-prescribed antimicrobials, the presence of challenges facing patients seeking antimicrobials without prescriptions, and pharmacists’ responses when they face patients without prescriptions. Consequently, it is essential to tackle the inappropriate use of antimicrobial agents alongside the insufficient understanding of their function in Jordan, with the objective of enhancing knowledge and practices related to antibiotic utilization among pharmacists and patients [
17].
3. Discussion
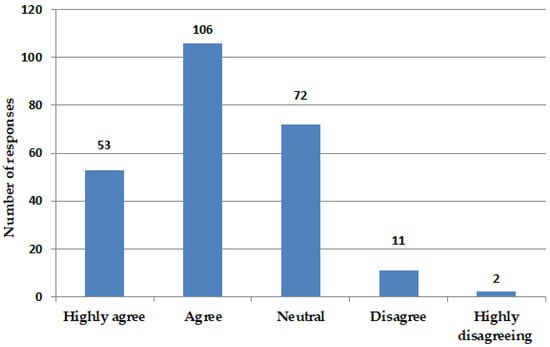
Antimicrobial resistance represents a growing public health challenge on a global scale. Pharmacists assume a critical function in the prescription of antimicrobials, attributable to their specialized knowledge in medication management and their availability to patients. A cross-sectional survey conducted among community scientists assessed their confidence levels in prescribing antimicrobials and the resources utilized to inform their prescribing decisions (159 out of 244,
Figure 1). A majority of pharmacists indicated a high level of confidence in the prescribing of antimicrobials. The resources most commonly utilized comprised clinical practice guidelines, as well as educational materials and training (
Figure 2). Pharmacists are strategically positioned to enhance antimicrobial stewardship through confident prescribing practices that are underpinned by dependable resources. Consistent participation in professional development and access to current clinical guidelines are essential for sustaining effective prescribing practices. The confidence of pharmacists in antimicrobial prescribing, coupled with the utilization of appropriate resources, significantly strengthens the efficacy of antimicrobial prescribing practices. It is imperative that pharmacists are provided with access to reliable information and continuous training to maintain effective prescribing practices and address the issue of antimicrobial resistance.
A significant proportion of pharmacists indicated that they often encounter patients who seek antimicrobials without prescriptions or rely on self-diagnosis for their requests. The aforementioned situations frequently result in the inappropriate use of antimicrobials, thereby exacerbating the growing issue of resistance. Furthermore, pharmacists encounter difficulties associated with incomplete medical histories and regulatory limitations, which further exacerbate the complexities of appropriate antimicrobial prescribing. The identified issues highlight the necessity for improved regulatory frameworks and educational initiatives aimed at bolstering pharmacists’ capacities in the prescribing of antimicrobials. There exists a pressing necessity for the implementation of policies aimed at dissuading self-medication and non-prescription requests, alongside the establishment of systems that guarantee pharmacists have access to comprehensive patient medical histories. It is imperative to address these challenges to mitigate antimicrobial misuse and combat resistance effectively. Accurate information is critical for the appropriate prescription of antimicrobials. Furthermore, a comprehensive understanding of patients’ medical histories is essential for the evaluation of their cases. The refusal to dispense antimicrobials presents challenges for pharmacists, representing considerable obstacles in the prescription process.
The non-prescription use of antimicrobial drugs, particularly antibiotics, raises significant concerns due to its potential contribution to the promotion of antimicrobial resistance. The use of ineffective pharmaceuticals or inappropriate dosages may elevate the likelihood of selecting prescriptions for resistant organisms that are challenging to eradicate [
16,
17].
The inappropriate use of antimicrobial agents has emerged as a significant global concern. A cross-sectional study conducted in Nigeria revealed that 60.7% (
n = 509) of consumers held the belief that antibiotics are effective against all infections, 57.4% lacked awareness regarding antibiotic resistance, and 72.5% reported having used antibiotics within the preceding 12 months [
18].
In a comparable investigation conducted in Pakistan, it was found that 39.2% (
n = 196) of participants had engaged in self-medication with antibiotics within the preceding six months, while 42% (
n = 207) exhibited non-adherence to their prescribed antibiotic treatment regimen [
19].
In Europe, despite the imposition of restrictions on non-prescriptive antibiotics, 50% (
n = 8221) of individuals reported having taken antibiotics within the preceding 12 months. Among these, 22% acquired antibiotics without a prescription, while 8% utilized leftover antibiotics. Furthermore, 84% of participants demonstrated a deficiency in understanding the proper use of antibiotics [
20].
A recent cross-sectional study conducted in the UAE revealed that 25.51% (
n = 1074) of participants had utilized antibiotics within the past 6 months, 24.21% within the past 12 months, and 19.18% had done so more than 12 months ago. Among the subjects surveyed, a mere 12% reported the use of non-prescribed antibiotics. Furthermore, 50% ceased treatment upon completion of the prescribed course, while 22.81% discontinued use when symptoms resolved. Additionally, 47.02% indicated that they stored unused antibiotics for future use, and 7.73% admitted to sharing these medications with family members [
21].
Clinical guidelines indicate that penicillin should be considered the primary treatment option for otitis media [
22]. It was observed that certain pharmacists opt to prescribe Macrolides as an alternative. In a comparable manner, established guidelines recommend the use of sulphonamides for the treatment of urinary tract infections (UTIs) [
23]; however, a subset of pharmacists choose to prescribe Fluoroquinolones instead. Such deviations may result in the misuse of antimicrobials, thereby fostering resistance and leading to less than optimal patient outcomes. The observed deviations can be attributed to potential miseducation or insufficient awareness of the current guidelines among pharmacists. Notwithstanding the existence of established guidelines, certain pharmacists may lack adequate familiarity with the current recommendations. The inappropriate use of antimicrobials resulting from non-adherence to clinical guidelines represents a significant concern that exacerbates the problem of antimicrobial resistance. By addressing the fundamental causes, including inadequate education and insufficient awareness, and by implementing targeted interventions, the prescribing practices of pharmacists can be harmonized with established clinical guidelines. The alignment in question is critical for the optimization of patient outcomes, the reduction in resistance, and the assurance of the effective utilization of antimicrobial agents.
Systematic protocols monitoring the prescribing and administrating of antimicrobials were approached and called “Antimicrobial stewardship” [
24]. The aim of this approach is to support and educate professionals in healthcare settings. Educated healthcare professionals will monitor the effectiveness of antimicrobial use. The effectiveness of antimicrobials use will improve patients’ outcomes and reduce the occurrence of antimicrobial resistance [
25]. In this investigation, the antimicrobial use indicated that antimicrobial stewardship must be followed to reduce antimicrobial resistance outcomes.
5. Conclusions
This study supports that antimicrobial resistance is a critical global health crisis fueled by inappropriate antimicrobial use, non-compliance with clinical guidelines, and self-medication. Pharmacists, key health providers, play a crucial role in addressing antimicrobial resistance through guideline-based prescribing, participation in antimicrobial stewardship programs, and patient education. Conversely, incomplete patient histories, insufficient awareness of guidelines, and regulatory shortcomings should be addressed for education improvement, stricter regulations, and improved access to medical information. Collaborative efforts are necessary to ensure the alignment of the established clinical protocols with prescribing practices, optimizing patient care and effectively tackling antimicrobial resistance.