1. Introduction
The diagnosis of nasal cavity disease (ND) can only reliably be obtained under anesthesia, ideally through a computed tomography (CT) of the head, endoscopy of the upper airways, histopathological examination of tumor biopsies, or nasal mucosa and mycological examination of mucosa swabs [
1,
2]. For diagnosing ND, the culture-dependent microbiological examination (ME) of a nasal swab was not helpful, as the frequency of positive culture and the type of bacteria are not significantly different among the various nasal diseases [
2]. Additionally, primary bacterial rhinitis in dogs is uncommon [
1] and not observed in recent studies using more comprehensive diagnostics [
2]. It should be noted that the nasal mucosa is physiologically colonized by bacteria [
3]. Even in nasal swabs of healthy dogs, 27 bacterial species were identified as normal flora by an anaerobic and aerobic cultivation of nasal cavity swabs [
3]. Detected bacteria in dogs with nasal discharge are believed to be secondary to another ND or commensal [
4,
5,
6,
7]. However, it has been suggested that bacteria may contribute to the worsening of primary diseases [
5], which is of therapeutic interest in dogs with idiopathic rhinitis (IR) of unknown etiology. The results of culture-based ME do not reliably display the bacterial profile that is detected by culture-independent sequencing methods [
5]. However, an early diagnosis and appropriate therapy of canine ND are urgently needed because first-line treatment with antibiotics is not indicated and may lead to a time delay or worsening of diseases (e.g., nasal tumors, mycotic diseases, foreign bodies) [
8].
Diagnostic examinations under anesthesia are costly, and owners might be afraid of the anesthetic risk, which is why there is a need for easy and inexpensive blood markers for diagnosing nasal cavity disease as well as for monitoring therapeutic success. Therefore, as the first part of a prospective trial, we described in a previous publication the blood values and ratios (e.g., neutrophil-to-lymphocyte ratio [NLR], albumin-to-globulin ratio [AGR], and the platelet-to-lymphocyte ratio [PLR]) [
9]. In this previous study, only the PLR was significantly higher in dogs with malignant ND than in those with benign ND or controls [
9]. These observations brought forward the question whether other additional serum inflammatory markers in dogs are related to ND and, as such, whether they may be utilized for diagnosis.
During inflammation and tumorigenesis, the concentrations of acute phase proteins (APPs), such as canine C-reactive protein (c-CRP) and haptoglobin (HPT), can increase [
10], while other serum biomarkers, such as 25(OH)D, may decrease [
11,
12]. In malignant tumors, increases in APPs may be caused by major inflammatory reactions due to infectious or non-infectious mild-to-severe inflammation, which has not been observed in benign neoplasia [
13]. Even if the acute phase response is generally short-lived, lasting just a few days, it supports the body’s innate immune defenses. In chronic inflammation, elevated concentrations of APPs have also been reported [
10]. A study of 48 dogs with ND revealed a significant difference between healthy dogs and dogs with ND in c-CRP as well as in HPT [
14]. Furthermore, significantly different levels were detected in HPT between dogs with rhinitis and aspergillosis [
14]. In humans, lower serum 25(OH)D concentrations were associated with a higher risk of respiratory infections [
15] and allergic rhinitis in children [
16]. The recent literature showed that 25(OH)D was significantly lower in dogs with sinonasal aspergillosis [
17].
After the diagnosis of IR, which is a diagnosis of exclusion after comprehensive diagnostics, treatment with doxycycline or macrolides may ameliorate clinical signs [
2,
18], although it is reported that these dogs in general respond poorly or only temporarily to antimicrobial treatment [
2,
18,
19,
20]. It is not clear whether the antimicrobial treatment of some kind of bacterial infection versus the immunomodulatory or anti-inflammatory effect (e.g., of doxycycline) is leading to a clinical improvement [
2,
7]. In some dogs, a good treatment response to corticosteroids or cyclosporine has been described [
19]. There are no general recommendations for the use of antibiotics in dogs with IR, which is especially of interest in the case of a positive-culture-based ME with a future therapeutic plan of anti-inflammatory agents (e.g., steroids). As c-CRP is used as a marker for a need for antibiotic treatment in humans with rhinosinusitis and suspected secondary bacterial infection [
21], we were interested in the utility of this marker in dogs with IR.
The aim of the present study was to evaluate the diagnostic utility of the serum biomarkers c-CRP, HPT, and 25(OH)D in dogs with ND. Our hypothesis was that these biomarkers would differ between dogs with malignant and benign ND, as well as between subgroups. Furthermore, the concentrations of these inflammatory markers were evaluated with regard to the result of the culture-based ME of a nasal cavity swab.
3. Results
In total, 55 of 72 dogs were included, comprising 13 dogs with nasal carcinomas, 12 dogs with nasal sarcomas, 7 dogs with benign nasal tumors, 13 dogs diagnosed with chronic IR, and 10 dogs with various benign inflammatory diseases, which were assigned to the “others” group (for diagnoses, see
Supplementary Table S1). In none of the 72 dogs with nasal disease was a primary bacterial rhinitis detected. Therefore, the group with malignant ND included 25/55 dogs (carcinomas and sarcomas; 45%), and the group with benign ND included 30/55 dogs (benign tumors, IR, and the other group; 55%) [
9]. The clinical nasal signs such as sneezing and/or nasal discharge in the 55 included dogs of the present study had been observed for a median duration of 5 months (IQR: 2–10). There were no statistically significant differences in the duration of clinical signs between the subgroups (carcinomas: median 6 months [IQR: 3–10.5], sarcomas: median 3.5 months [2–7.5], benign tumors: median 5 months [IQR: 4–7], IR: median 8 months [IQR: 2–18], other: 3 months [IQR: 1.4–7.5]). The inflammatory serum markers c-CRP, HPT, and 25(OH)D were recorded for all subgroups (
Table 1).
3.1. Correlation between the Serum Inflammatory Markers
A significant negative correlation was detected between c-CRP and 25(OH)D (negative correlation; rs = −0.273;
p = 0.044). The comparison of the concentrations of the inflammatory markers in the present study with the previously calculated NLR [
9] revealed a significant positive correlation of the NLR and c-CRP (rs = 0.404;
p = 0.003).
3.2. Haptoglobin
HPT concentrations (all values in the reference interval up to 3 g/L;
Table 1) were not significantly different among dogs with nasal cavity disease (median: 1.6; IQR: 1.1–1.8 g/L) or among the different groups compared with control dogs (median: 1.4; IQR: 0.3–1.7 g/L).
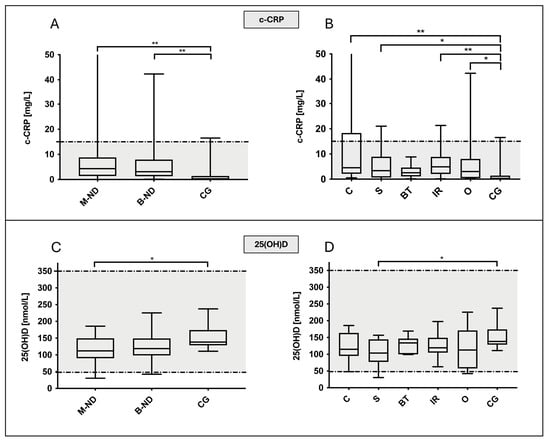
3.3. 25-Hydroxyvitamin-D
Median 25(OH)D concentrations of the different groups were within the reference interval of 48–350 nmol/L, except for two single values that were below the reference interval (one dog with nasal sarcoma at 30.3 nmol/L and one dog of the others group with 42.4 nmol/L,
Table 1). The 25(OH)D concentrations were significantly lower (
p = 0.041) in dogs with ND (median: 118, IQR: 94.6–149.3 nmol/L) than in controls (median: 138.4, IQR: 128.7–174.3 nmol/L;
Figure 1). While no significant difference was detected between control animals and dogs with benign ND (median: 119, IQR: 98.6–149.3 nmol/L), compared to control dogs, 25(OH)D was significantly decreased in dogs with malignant ND (median: 112, IQR: 90.3–149.5 nmol/L;
p = 0.041). Dogs with sarcomas, but not dogs with carcinomas, had significantly lower 25(OH)D levels compared to CG (
p = 0.025).
3.4. Canine C-Reactive Protein
The median c-CRP values of the different groups were within the reference interval below 15 mg/L, except for single values per group (
Table 1). However, c-CRP was significantly higher in dogs with ND in general (median: 4.1; IQR: 1.4–7.9 mg/L) compared to controls (median: 0.2; IQR: 0–1.4 mg/L;
p = 0.001;
Figure 1). Similarly, c-CRP values of dogs with malignant (median: 4.3; IQR: 1.4–8.8 mg/L;
p = 0.002) and benign ND (median: 3.1; IQR: 1.3–8 mg/L;
p = 0.006) were both significantly increased compared to the control group, although they were not significantly different from each other. Further subgroup comparisons showed significantly higher c-CRP concentrations in dogs with nasal carcinomas (
p = 0.002) and IR (
p = 0.009) than in the control group but also in dogs with nasal sarcomas (
p = 0.031) and in those of the others group (
p = 0.033). Compared to the CG, c-CRP levels in dogs with benign tumors were not significantly increased.
3.5. Culture-Dependent Microbiological Examination
Antibiotic history was available for 54 of 55 dogs. Antibiotic pre-treatment for nasal disease was reported in 40/54 dogs (74.1%;
Figure 2A)—with 13/13 dogs of the IR group, 13/24 dogs with malignant tumor (in one dog, information was not available [n.a.]), 10/10 dogs of the others group, and 4/7 dogs of the group with a benign tumor (
Figure 2A). The administered antibiotics were amoxicillin clavulanic acid (n = 10), amoxicillin (n = 4), doxycycline (n = 8), unknown antibiotic (n = 11), enrofloxacin (n = 2), marbofloxacin (n = 5), and cefalexin and clindamycin in one dog each.
A positive culture-dependent ME was reported in 11/21 dogs (44%) with malignant nasal tumors (sarcomas and carcinomas; information was not available [n.a.] in four dogs including one dog with a pre-reported negative ME) and in 8/13 IR dogs (61.5%). In benign tumors, only 1/7 dogs (14.3%) had a positive ME and only 3/10 dogs (30%) in the others group (in 2 of 3 dogs with
Aspergillus spp., infection ME was negative;
Figure 2A).
The effect of antibiotic pre-treatment on the result of ME was evaluated, after excluding dogs with positive results for Aspergillus spp. in combination with a negative ME due to an unknown influence of Aspergillus spp. on the ME result, as well as the dogs for which no ME result was available. There was no statistically significant correlation between pre-treatment with antibiotics and the negativity of ME between dogs that had received antibiotics less than 4 weeks prior to presentation (9/54 dogs, 4 positive and 5 negative ME) and dogs that had received antibiotics more than 4 weeks prior to presentation (27/54 dogs, 14 positive and 13 negative ME; chi-square test, p = 0.819). Additionally, there was no statistical difference between these pretreated dogs that had received antibiotics in general (n = 36, 18 positive and 18 negative ME) and the dogs without pre-treatment with antibiotics (n = 12, 5 positive and 7 negative ME; chi-square test, p = 0.617).
Cultivated bacteria did not differ significantly in various nasal diseases. They are shown in
Figure 2B–D, with
S. intermedius most often cultivated in dogs with malignant nasal tumors. Serum c-CRP values were not statistically different in dogs with distinct detected bacteria such as, e.g.,
Pasteurella multocida or
Staphylococcus aureus.
The positivity of ME revealed no significant differences in the above-mentioned biomarkers (data are exemplarily shown for c-CRP in
Figure 3A). Even if median c-CRP concentrations were higher in dogs with positive ME in the groups malignant tumor (
p = 0.63), idiopathic rhinitis (
p > 0.99), and others (
p = 0.25), there was no statistically significant difference.
3.6. Excluded Dogs
In total, 17 of 72 dogs were excluded after workup for nasal cavity disease due to, e.g., one or more of the following recognized diseases or due to actual treatment with steroids (n = 5) for one of these underlying chronic diseases. Systemic diseases included polyarthritis or osteoarthritis (n = 5), pulmonary fibrosis, infectious/bacterial pneumonia (n = 2, one dog was diagnosed based on bronchoalveolar lavage results and another based on the clinical signs of fever and pneumonia responsive to antibiotics), mast cell tumor, tumor ventral to the urinary bladder, leishmaniasis (n = 2), structural abnormalities of the liver parenchyma (n = 3), hepatic shunt, chronic pancreatitis, acute gastroenteritis, inflammatory bowel disease, and protein-losing enteropathy. Excluded dogs would have been assigned to the following groups with respect to nasal cavity disease: five dogs in the idiopathic rhinitis group, six dogs in the others group (3/6 dogs with primary SNA), three dogs in the malignant nasal tumor group, and one dog in the benign tumor group. In two dogs, nasal signs were most likely due to rhinitis secondary to the systemic disease of leishmaniasis and, therefore, would not have been categorized into any of the local nasal cavity disease groups.
In general, the c-CRP values of the excluded dogs (see
Table 1) were not elevated, with the exception of six dogs (two IR dogs with lung disease, one of the others group with dental disease and lung disease, one dog with malignant nasal tumor in addition to suspected metastases, one dog with benign tumor due to a high-grade oronasal fistula, and one dog with leishmaniasis). Canine CRP concentrations were not significantly increased in this group of dogs in contrast to dogs with nasal cavity diseases but from healthy dogs (Kruskal–Wallis test;
p = 0.0045;
Table 1). Haptoglobin and 25(OH)D concentrations were within the reference interval in all dogs according to our external laboratory and did not differ statistically significantly from dogs with nasal cavity disease or controls (
Table 1).
The following information can be emphasized in the context of the subsequent discussion of the results. The three dogs with primary SNA were excluded due to polyarthritis in addition to permanent treatment with prednisolone, due to a lack of whole-body CT or severe osteoarthritis under treatment with mavacoxib. In all three dogs, no increased c-CRP (6.9 mg/L, 8.5 mg/L, and 4.3 mg/L) or haptoglobin (1.45 g/L, 1.14 g/L, and 1.28 g/L) was detected, which is comparable to the results in the dogs of the others group. However, the 25(OH)D concentrations were low (125.8 nmol/L, 53.47 nmol/L, and 52.48 nmol/L).
The five dogs with idiopathic rhinitis were excluded because three of them had lung disease (infectious pneumonia n = 2 and pulmonary fibrosis n = 1), the fourth had inflammatory bowel disease in addition to previous treatment with corticosteroids, and the fifth had pancreatitis in addition to abnormalities of the liver parenchyma. In both dogs with infectious pneumonia, c-CRP was increased at 38.4 mg/L and 25.5 mg/L, respectively, in contrast to the other three IR dogs, in which c-CRP was 0 in the dog with liver abnormalities or in the reference interval (n = 2). Haptoglobin was in the reference interval (1.42 g/L and 1.86 g/L) in the two dogs with pneumonia, as well as in the other IR dogs, as was 25(OH)D.
3.7. T-Category of Nasal Tumors
Furthermore, as there was no significant difference between marker concentrations and tumor type, markers were evaluated in regard to tumor size (T-category; T1 to T3 versus T4 with cribriform plate lysis) in malignant tumors. Although there were higher median values in c-CRP in carcinomas and sarcomas in T-category 4 noted, they were not significantly different (carcinomas:
p = 0.093; sarcomas:
p = 0.497;
Figure 3B). For the reason of completeness, evaluating the influence of tumor size on c-CRP concentrations,
Figure 3B shows values of benign tumors, which, however, only had a size up to T-category 3.
3.8. Histopathological Examination
Lymphoplasmacytic inflammation was seen in some dogs with IR but also in one dog with oronasal defect (
Figure 4A). Neutrophilic inflammation was mostly observed in dogs with IR. In these dogs, the ME was negative and c-CRP within the reference interval (
Figure 4). Numerically higher c-CRP values were noted in dogs with lymphoplasmacytic inflammation (not significantly different).
4. Discussion
The acute phase proteins c-CRP and HPT and the serum marker 25(OH)D were not significantly different among the groups of dogs with ND in the present study. Therefore, they appear to not be clinically useful for the reliable detection or therapy monitoring of ND in dogs. This result is in line with one previous study in which no high-grade abnormalities in the blood count or blood chemistry in general or between the different groups of dogs with ND were detected [
9]. Regarding blood ratios, only the platelet-to-lymphocyte ratio (PLR) was significantly higher in dogs with malignant nasal cavity tumors compared to dogs with benign, inflammatory diseases or to control dogs [
9].
In the present study, the c-CRP median value of dogs with ND in general of 4.1 mg/L [IQR: 1.4–7.9] was overall in the reference interval with only individual values outside the upper reference limit of 15 mg/L. Therefore, the median c-CRP level of this present study was lower than in another study of c-CRP concentrations in canine ND (aspergillosis: median: 13.4 [IQR: 2–82]; rhinitis: median: 4.8 [IQR: 1–44]; neoplasia: median: 14.8 [IQR: <0.78–69]; healthy dogs: median: 1.5 [IQR: <0.78–9.6]) [
14]. The reason for the difference in c-CRP concentrations in both studies could be the measuring method [
29]. In the cited study, an immunoturbidimetric assay for canine CRP on a MIRA (Roche Diagnostics) was used [
14,
30,
31] compared to the Gentian canine CRP immunoturbidimetric assay used in this present study [
24,
25,
26,
27]. Another reason for the different c-CRP concentrations in dogs with nasal cavity diseases in the two studies could be additional or underlying undetected diseases in the dogs included in the cited study [
14]. However, based on the data of the present study, we can conclude that c-CRP levels are not extremely increased in dogs with ND. One reason could be that dogs with nasal cavity diseases are most often not presented in the acute phase but in the late course of the disease (in the present study, the median duration of nasal signs in the 55 included dogs was 5 months [IQR: 2–10]). However, it should be noted that an increase in APPs has also been described under chronic inflammation [
10,
32]. Another reason could be that ND in dogs does not result in a significant acute phase response, which is what has to be evaluated in further studies evaluating the APPs in dogs with acute clinical nasal signs. Canine CRP, therefore, still can be used for the monitoring of the therapy response of additional or subsequent diseases where c-CRP values are much higher and where c-CRP has been proven as a reliable marker for therapy response. Examples are sepsis [
33], SRMA [
33], or bronchopneumonia (e.g., with c-CRP: 121 mg/L [IQR 68–178 mg/L]) [
34]. This is clinically helpful, as it is known that the aspiration of nasal secretions and secondary bronchopneumonia may occur consequently in dogs with idiopathic rhinosinusitis. Two excluded dogs of the present study with IR (long-term clinical signs of nasal cavity disease) and acute clinical signs of bacterial pneumonia showed increased c-CRP concentrations, supporting this hypothesis.
As reported before, this present study proved that a high number of positive culture-dependent MEs was obtained in the different groups of dogs with nasal cavity disease and that there were no differences between bacterial species [
2]. The results of the ME are, therefore, not diagnostic in dogs with ND. According to the literature, the highest number of positive MEs was obtained in the group IR [
2]. Additionally, in dogs with malignant nasal tumors,
S. intermedius was cultivated most frequently [
2].
Since the use of conventional antibiotics does not lead to long-term therapeutic success in dogs with IR [
20], the use of antibiotics in some IR dogs is being discussed. In human medicine, even though in 60% of patients with acute rhinosinusitis bacteria are detected, most cases resolve spontaneously [
21]. Additionally, CRP has been shown to be a useful test for the diagnosis of bacterial sinusitis in humans and helped to reduce antibiotic prescriptions in patients with acute rhinosinusitis [
21]. This diagnostic benefit could not be verified in the present study for dogs with IR, as the c-CRP value recorded in this study did not statistically significantly differ between dogs with positive and negative ME. A limitation, however, is the small number of dogs with IR and thus with positive ME, which is why a larger number of dogs with IR has to be evaluated after the exclusion of secondary bronchopneumonia or other diseases in order to prove this result.
The type of mucosa inflammation in IR dogs or the size of malignant and benign tumors in the dogs of the present study were discussed by the authors of the present study as additional influencing factors on the serum concentration of c-CRP. Interestingly, c-CRP concentrations were numerically higher in lymphoplasmacytic rhinitis than in neutrophilic. However, the number of animals is too small to conclusively prove this finding. Regarding tumor size, classification into T-categories can be helpful to establish a prognosis and is, therefore, important for the owners in terms of treatment expectations after radiation therapy [
22]. As cribriform plate lysis is not always easy to detect, it is interesting that some c-CRP values were observed to be higher in dogs with T4 nasal tumors with cribriform plate lysis. Therefore, this marker could potentially be helpful in detecting or monitoring dogs of the T4 category. Due to the small number of dogs with the T4 category, further studies are needed to evaluate the c-CRP values in a larger group of these dogs.
The serum concentrations of the HPT of dogs in this study were within the reference interval of 0–3 g/L and were not significantly different among the different ND groups. This contradicts other findings, where HPT levels were significantly different between dogs with nasal discharge and healthy dogs as well as between dogs with aspergillosis and rhinitis [
14]. The median values in the aforementioned study were higher than in the present study, with the median for aspergillosis at 5.2 g/L (IQR: 2–19.2), for rhinitis at 2.9 g/L (IQR: 0.8–5.8), for neoplasia at 4.1 g/L (IQR: 0.3–10.8), and in healthy dogs at 0.65 g/L (IQR: <0.02–4.3) [
14]. The results of the present study may have been influenced by the measuring method. The cited study used an haptoglobin-hemoglobin-binding capacity assay [
14,
35] in contrast to the Tridelta PHASE Haptoglobin Assay [
28] used in the present study. Other factors influencing the haptoglobin concentrations in the present study could have been the exclusion of dogs with additional diseases and the lower number of dogs with aspergillosis (3 dogs compared to the 13 dogs in the cited study) [
14]. Furthermore, HPT could have been lower in the present study as dogs were excluded if pretreated with steroids 14 days before presentation in contrast to 7 days in the other study. Corticosteroids are reported to increase HPT concentrations [
36], which has not been described for other APPs [
10,
36].
Circulating metabolite 25(OH)D is an indicator of vitamin D concentrations and plays an important role in the immune system [
16]. The interpretation of serum concentrations may be difficult as the levels of 25(OH)D can vary widely in dogs [
37]. Furthermore, its concentration is mainly determined by the amount of vitamin D intake through the diet, since dogs cannot adequately produce vitamin D3 in their skin under UV light [
11,
12]. Therefore, decreased 25(OH)D concentrations have been detected in dogs with various diseases, such as, e.g., chronic kidney disease, heart failure, inflammatory bowel disease, and mast cell tumors [
11,
12]. Interesting for the present study, recently, decreased concentrations have been detected in shelter dogs with infectious respiratory disease complex [
38], as well as in dogs with sinonasal aspergillosis [
17].
There was no significant difference in 25(OH)D concentrations between dogs with different NDs in this study. However, compared to the healthy control dogs, significantly lower 25(OH)D levels were detected in dogs with malignant tumors, especially sarcomas. This is in line with the literature, as 25(OH)D is discussed as a precursor of 1.25-dihydroxyvitamin D in tumorigenesis in humans [
39,
40], and, as in dogs with lower 25(OH)D concentrations, the relative risk of cancer was increased [
37]. If vitamin D insufficiency is confirmed in further studies with larger numbers of dogs, vitamin D supplementation could possibly also prove useful in dogs with nasal tumors as supplementation is suggested to increase the responsiveness of cancer cells to chemotherapy [
37] and to inhibit tumor cell growth [
41]. Nevertheless, systemic vitamin D supplements for tumor therapy and prevention should be performed with caution, as it is associated with a risk of hypercalcemia [
39,
41].
Even if in the present study all 25(OH)D values were still within the reference interval of our external laboratory, all dogs showed concentrations beneath 250 nmol/L (=100 ng/mL). In the literature, 250 nmol/L was considered to be the minimum for vitamin D sufficiency (using a direct, competitive 25(OH)D chemiluminescence immunoassay and serum samples) via simultaneous measurements of intact parathyroid hormone [
37] with deficient levels < 75 nmol/L (=30 ng/mL), insufficient concentrations with values between 75 and 250 nmol/L (=30–100 ng/mL), and sufficient levels above 250 nmol/L [
37]. According to these data, all dogs in the present study, including controls, showed 25(OH)D insufficiency. Furthermore, 11 dogs with nasal disease (11/55; 20%) were deficient, with values < 75 nmol/L (two carcinomas, three sarcomas, two IR, and four others). One limitation is the low number of dogs with SNA, which is why 25(OH)D could not be examined separately in this group of dogs.
However, if we would not have had to rule out the three dogs with primary SNA due to the above-mentioned limitations, and if we calculate the concentrations of the serum marker separately for all six dogs with SNA (three excluded primary SNA, two secondary SNA, and one primary SNA of the others group), the c-CRP (median 5.6 [IQR: 3.1–17.0]) and haptoglobin (median 1.4 [IQR 1.1–1.9]) concentrations were not statistically significantly different as were the 25(OH)D concentrations. However, in accordance with another study [
17], the 25(OH)D concentrations appeared numerically low, with a median of 57.1 [IQR 51.9–150.7]. Therefore, further studies are needed to evaluate this finding in dogs with SNA.
The exact reasons for these low 25(OH)D concentrations in the present study, apart from the disease itself, cannot be given here. Another study also showed significant differences in 25(OH)D concentrations in apparently healthy dogs, with a few showing very low concentrations [
37]. The control dogs in the present study were experimental dogs with a standardized diet, which may have had an influence here, but this cannot be determined retrospectively due to a lack of food analyses.
As with c-CRP and haptoglobin, differences in 25(OH)D concentrations may also be due to the measurement method. Although the measurement method used here was validated in the external laboratory for canine samples, there are no published studies in dogs that used this method and could be used for the comparison of concentrations.
In this study, we observed a negative correlation between c-CRP and 25(OH)D. This result is comparable to findings in humans, where it was shown that in addition to an increase in c-CRP, a reciprocal decrease in 25(OH)D may be observed [
42,
43,
44]. Therefore, 25(OH)D was described as a negative acute-phase factor [
42,
43,
44].
In the present study, nasal cavity diseases were diagnosed using standardized, comprehensive diagnostics. Dogs with other obvious diseases except the nasal cavity following whole-body CT with contrast and blood tests possibly influencing marker concentrations were excluded. It can be considered a limitation, as discussed before, that because the acute phase response is a rapidly occurring, non-specific reaction to an inflammatory stimulus, taking place even before the clinical signs of disease appear, significantly different initial changes in the included dogs may have been missed even if an increase in APPs has also been described under chronic inflammation [
10,
32]. As a further limitation, all dogs with nasal discharge were recruited at a tertiary institution, and selection bias cannot be excluded. To date, no significant influence of age, breed, or sex on the concentration of APPs has been found [
10], which is why gender and age differences in the examined groups were not assumed to influence the results.