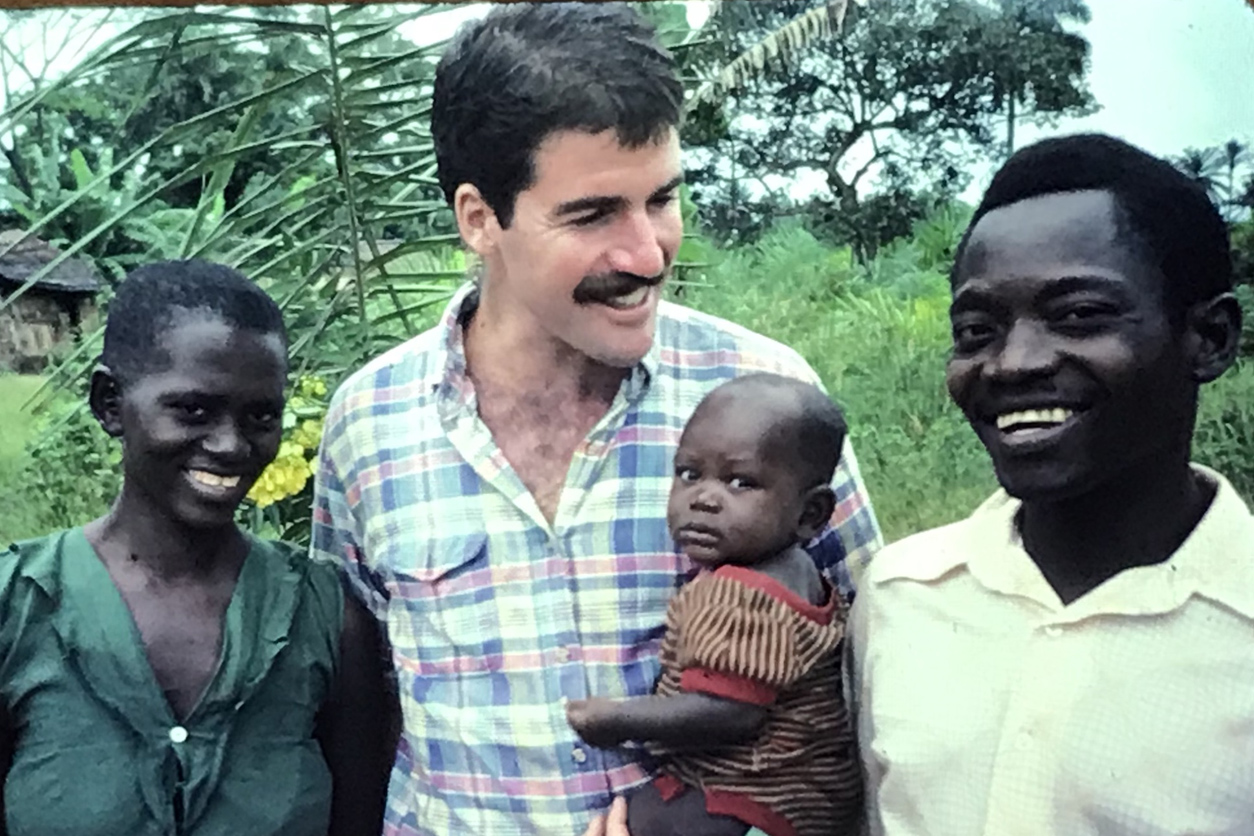
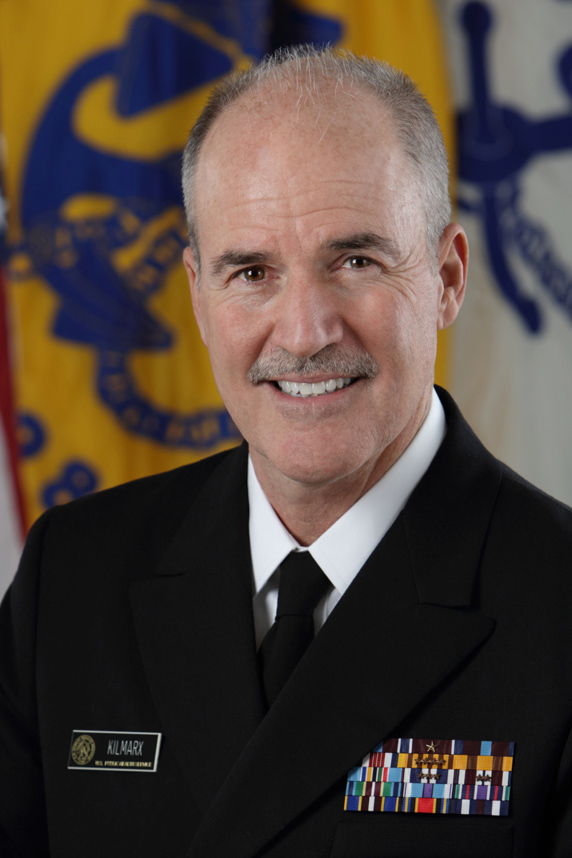
I recently sat down with Peter Kilmarx, M.D., acting director of the NIH Fogarty International Center (FIC), to discuss adaptation science, a critical yet often overlooked area in the broader conversation on climate change. As climate-related environmental challenges and extreme weather events continue to intensify, adaptation science — which is about understanding and implementing strategies to strengthen health and resiliency — becomes paramount.
Also, health threats posed by climate change are global in nature, so fostering international scientific collaboration — central to the mission of FIC — is critical. That is one reason why I am excited to share excerpts of my talk with Dr. Kilmarx, as he brings a wealth of experience and knowledge on how to build effective global partnerships. For me, the conversation served as a strong reminder of the interconnectedness of climate change and human health, and the role of multidisciplinary science in helping people everywhere to improve health outcomes.
As Dr. Kilmarx aptly noted, “Adaptation science is about looking forward, anticipating the challenges ahead, and equipping ourselves with the knowledge and tools to face them.” Climate change can impact our lives in numerous complex ways, so embracing adaptation science is essential for ensuring that the approaches individuals and communities adopt account for that complexity. Through research and greater collaboration, we can advance adaptation strategies that help people in the U.S. and around the world to live healthier lives.
Expanding research partnerships
Rick Woychik: Let’s kick things off by first talking about the Fogarty International Center and your major focus areas.
Peter Kilmarx: Sure. The Fogarty International Center is the smallest of the NIH institutes and centers based on our budget and staffing, but we have a very big mission, which is to support all of NIH in its global research activities. We focus especially on training and capacity building in lower income countries to expand scientific partnerships between those countries and NIH, and we work a lot in infectious diseases and noncommunicable diseases.
It is not often appreciated that NIH is in fact a global enterprise. A few years ago, we found that there are about 80,000 scientific publications each year that cite NIH funding, and 35% of those publications have coauthors outside of the U.S. We discovered that those publications actually have a higher scientific impact factor compared with those with only U.S. authors.
Climate change and health
RW: Fogarty was among the first NIH institutes and centers to actively participate in the NIH Climate Change and Health Initiative, which NIEHS is helping to lead. Can you elaborate on Fogarty’s interest in this area?
PK: Climate change is certainly a focus at Fogarty because it represents a significant health threat on a global scale. There’s a scientific imperative to learn more about how it will affect us and to discover what we can do to minimize the negative impacts. That kind of research requires a multidisciplinary approach, and it involves almost every NIH institute’s scientific interest.
Fogarty has played a role in supporting and coordinating research efforts related to climate change involving multiple institutes and centers, such as through our Global Environmental and Occupational Health Program, which NIEHS has participated in. I should add that the social justice aspect of climate change — where lower income countries face the greatest impacts — resonates with Fogarty’s mission, and we are committed to addressing these disparities.
Extreme weather’s direct and indirect effects
RW: What are some of the direct and indirect effects of climate change that you think will require increased research moving forward?
PK: Direct effects, such as injuries, infectious diseases, and mental health issues, can stem from extreme weather events like cyclones and flooding, where massive loss of live can devastate families and entire communities. Extreme conditions also pose risks to agricultural and factory workers through heat exhaustion, stroke, and acute kidney injuries. Furthermore, climate change is altering disease vectors, introducing infectious diseases to new regions.
Indirect consequences include things like destruction of healthcare infrastructure by hurricanes, where patients who depend on ongoing treatments such as dialysis or chemotherapy find their care networks disrupted. Moreover, climate change is exacerbating migration and refugee crises, with people fleeing their homes due to droughts and storms. These shifts have profound impacts on mental health, contributing to climate anxiety and other concerns.
Adaptation science
RW: What exactly is adaptation science? And how does it differ from climate mitigation?
PK: While there’s some overlap between the two, mitigation tends to focus on prevention of climate change, and adaptation tends to emphasize managing its impact.
Mitigation involves reducing emissions or increasing absorption of greenhouse gases, encompassing strategies from renewable energy to changes in transportation and diet. Adaptation acknowledges the reality of climate change, focusing on adjustments to minimize its effects through a variety of strategies, including biomedical, behavioral, and structural changes.
Adaptation strategies are as varied as the direct and indirect challenges we just discussed. For outdoor workers, simple measures like providing rest, shade, and hydration can significantly reduce the risk of acute kidney injury. But many seemingly beneficial proposed strategies will require careful health impact evaluations and research moving forward.
Understanding unintended consequences
RW: Can you expand on that?
PK: Consider the practice of rainwater collection to combat the effects of drought. While beneficial for hydration and hygiene, that can create breeding grounds for disease vectors like mosquitoes, leading to increased Dengue fever incidence.
Similarly, while indoor air filters can combat wildfire smoke by reducing levels of fine particulate matter, their impact on specific health conditions like chronic obstructive pulmonary disease or asthma has not been fully assessed.
There can even be unintended consequences of tree planting, particularly regarding pollen and allergies. While planting trees is generally seen as a beneficial action for carbon capture and urban cooling, the resulting increase in pollen can exacerbate allergies for many people. This illustrates the importance of selecting low-allergenic trees and considering health outcomes like allergy-related medical visits when planning urban greening projects.
The point here is that as scientists, we must consider the broader implications of our proposals, including potential risks. At NIH, I believe we have a strong role to play in terms of enhancing health outcomes through careful study and implementation of these interventions.
More collaboration on the horizon
RW: Any closing thoughts for our readers?
PK: I would just add that when it comes to improving health outcomes in the face of climate change, both adaptation science and mitigation efforts are important.
Adaptation science allows us to understand and anticipate the impacts of climate change on diverse ecosystems and human populations, enabling us to prepare and respond more effectively. And mitigation efforts are essential, too, because they address the root causes of climate change, primarily through the reduction of greenhouse gas emissions.
Finally, the importance of scientific collaboration cannot be overstated. It is through sharing knowledge, resources, and technologies that we can accelerate innovation and scale up effective interventions grounded in best practices and the latest research. That is one reason why we at Fogarty are excited to collaborate with NIEHS and other NIH institutes on the Climate Change and Health Initiative, and we look forward to fostering fruitful partnerships with your institute and other organizations in the years ahead.
Source link
factor.niehs.nih.gov

