“Healthy babies start with healthy gametes,” said NIEHS grantee Richard Pilsner, Ph.D., and men have a 74-day window to get it right.
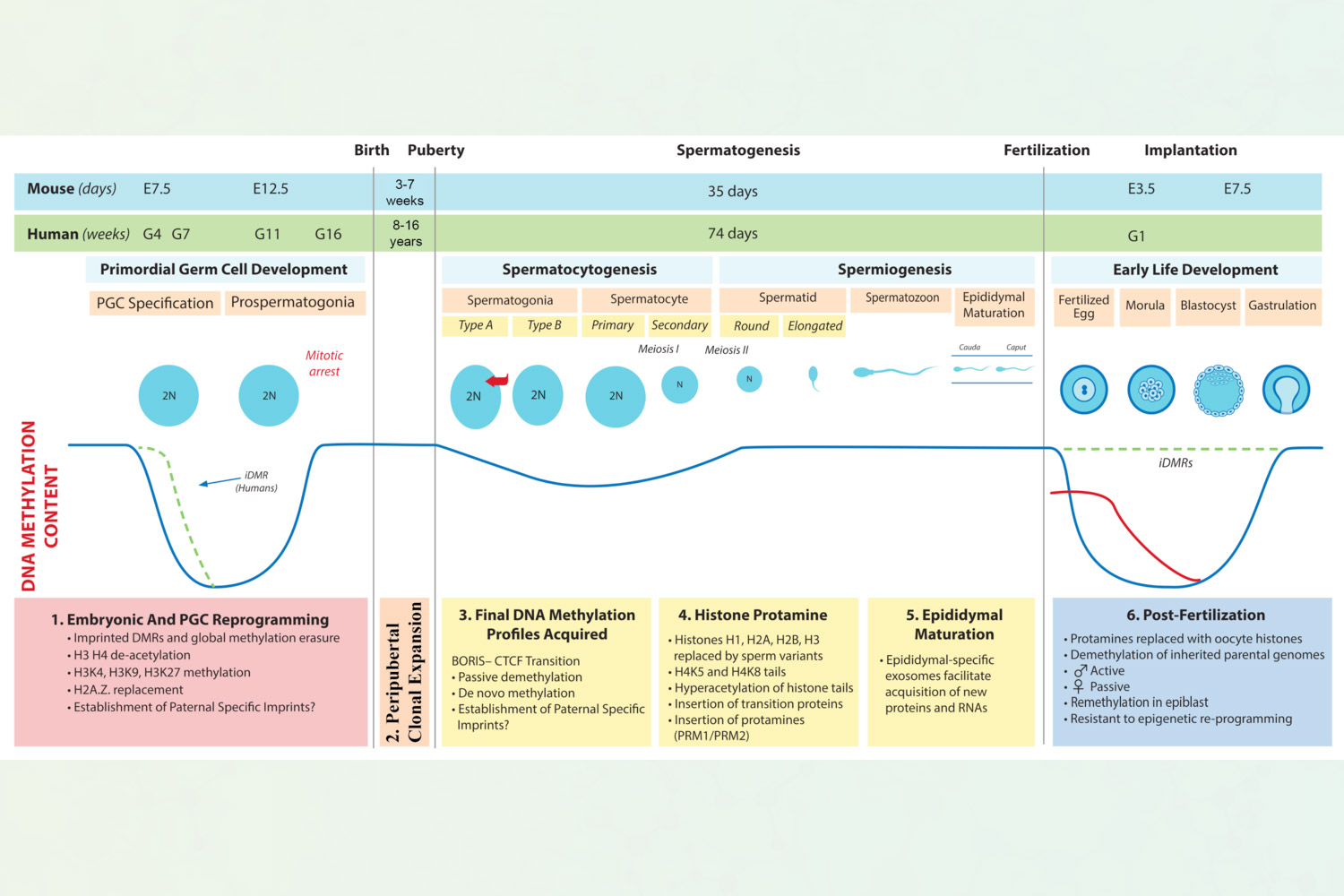
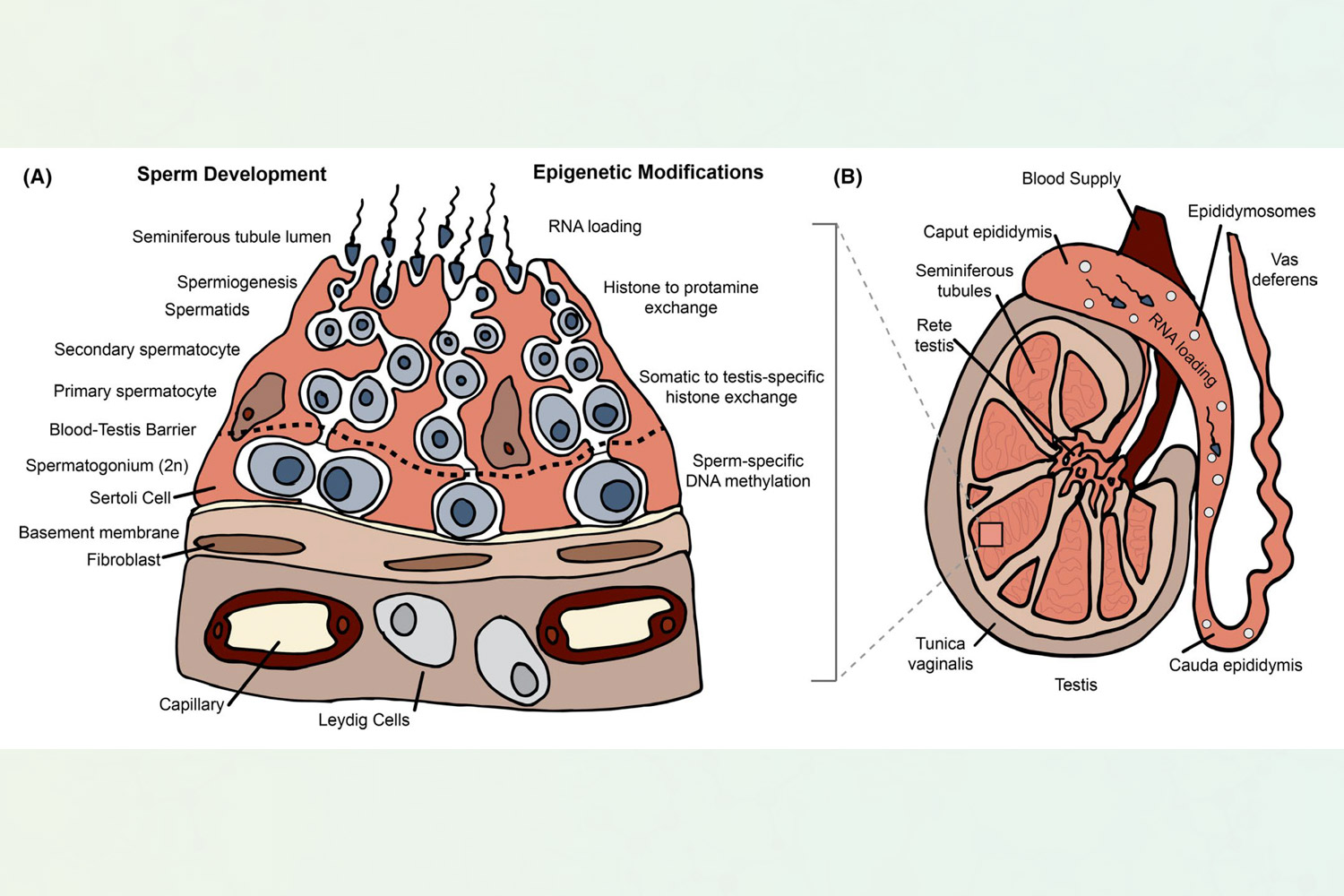
However, before a male gamete, or sperm, is fully developed, it undergoes epigenetic changes, which turn on or off individual genes. This is the sweet spot, when men should avoid environmental exposures for the best reproductive outcomes, according to Pilsner. He is a Robert J. Sokol, M.D., Endowed Chair of Molecular Obstetrics and Gynecology, and member of the Institute of Environmental Health Sciences at Wayne State University.
It takes two
When Pilsner graduated from Columbia University in 2007, he and his wife-to-be moved to Ann Arbor for his postdoctoral fellowship at the University of Michigan. They began talking about starting a family. Being a toxicologist, Pilsner mentioned that she should avoid alcohol, stay away from pesticides, and make sure she was eating healthy.
“You know, I began listing all the things she should be careful about, and my wife, who is a strong New York woman, turned to me without missing a beat and asked, ‘And what about you?’”
“I thought, ‘Why me?’ Then, about two weeks later, I had some downtime in my office — I remember it very clearly — and I thought, ‘Huh, sperm epigenetics? Let me look into this.’”
Thus, Pilsner’s research trajectory was born.
It was not an easy seed to sow. “I got slammed by reviewers,” Pilsner recalled. “The dogma at that time was all the methylation patterns were already set in sperm in utero and were not modified during spermatogenesis [the process of sperm maturation] in the adult male.”
Lucky for Pilsner, other researchers were discovering how exposures in animal studies affected offspring.
Pilsner responded to reviewers with an explanation of how these new discoveries would help him to explore such phenomena in humans. Funding was approved, and the Pilsner Lab got to work.
Windows of opportunity
It takes 74 days for the spermatogenesis cycle to be completed, and during those 74 days, it is important for men to reduce environmental exposures.
“Environmental exposures during that 74-day window could influence those final epigenetic patterns,” Pilsner said. “Subsequently, that can influence reproductive success, and potentially offspring health and development as well.”
So, Pilsner’s wife was right.
“The preconception window has been overlooked,” he said. “Men have an environmental responsibility that starts at a minimum of 74 days before conception. So, when couples are thinking about planning for pregnancy, it is not just the female that has to get ready. Males have to get ready as well, and that preparation should begin at least three months prior to conception.”
Everything women are told to avoid during preconception and pregnancy — from drinking alcohol and smoking (both tobacco and marijuana) to poor diet and no exercise — are not ideal on the male side of the conception process either, according to Pilsner.
In addition, phthalates are a common environmental exposure (see sidebar), which when present in high concentrations in the body have been associated with sperm epigenetic profiles in biological pathways known to be important for early embryonic development.
“Most of the phthalates that are associated with these sperm epigenetic changes in our human studies are considered anti-androgenic, meaning that they interfere with normal hormone production,” Pilsner explained. “To corroborate our findings in humans, preconception phthalate exposure in male mice revealed that phthalates were driving the expression of key developmental genes early in embryo development.”
How old is sperm, really?
Aging, and not just timing of exposure, is another significant topic in this discussion.
“We developed an epigenetic clock specific to sperm,” Pilsner explained. “This epigenetic clock measures the predicted biological age of sperm instead of chronological age.”
If there was a mismatch between chronological age and biological age (for example, the male is 25 years old, and his sperm is that of a 30-year-old), that couple is going to have a harder time getting pregnant. In fact, there is a 17% lower probability of pregnancy in couples where the man has an “older” rather than “younger” sperm age.
Moreover, phthalate exposure is associated with increased sperm epigenetic age. Pilsner’s lab is now looking into other types of exposures, as well as exposure mixtures, to identify additional environmental factors that affect male reproductive health.
It is important to note that sperm is only a small fraction of the total semen sample. The majority is seminal plasma, which is enriched in extracellular vesicles. These small membrane-bound vesicles secreted from cells aid in cell-to-cell communication by providing nucleic acid and protein cargo from donor-to-recipient cells.
Recent research from Pilsner’s lab has identified noncoding RNA profiles found in seminal plasma extracellular vesicles that were associated with both male infertility and phthalate exposure.
(Jennifer Harker, Ph.D., is a technical writer-editor in the NIEHS Office of Communications and Public Liaison.)
Source link
factor.niehs.nih.gov

