“Transforming Communities by Enhancing Women’s Health” was the theme of the eighth annual NIEHS Women’s Health Awareness (WHA) conference, which was held on April 9 and drew more than 1,100 registrants from across the U.S. The conference featured 23 virtual health sessions, exhibitor resources, and health demonstrations.
“Today, we celebrate eight years of improving health awareness, environmental public health outcomes, and health literacy among women,” said Joan Packenham, Ph.D., director of the NIEHS Office of Human Research and Community Engagement and the WHA Program. “We hope that during this conference, you will learn important health information that will positively impact your daily life. Our goal is to promote healthier lives through environmentally safer homes and communities.”
Bringing health to all communities
New this year was an innovative Strive to Thrive health video series demonstrating preventative health skills, allowing individuals to monitor and improve their health. Also, health equity and access were focal points throughout the conference.
To provide viewing access to women in rural communities where Wi-Fi connections are limited, two public satellite sites were set up in Granville and Haywood counties, both in North Carolina.
“We heard the voices of many women from rural North Carolina communities that they felt left out, disconnected, and needed access to the programming that Women’s Health Awareness provides,” said Packenham.
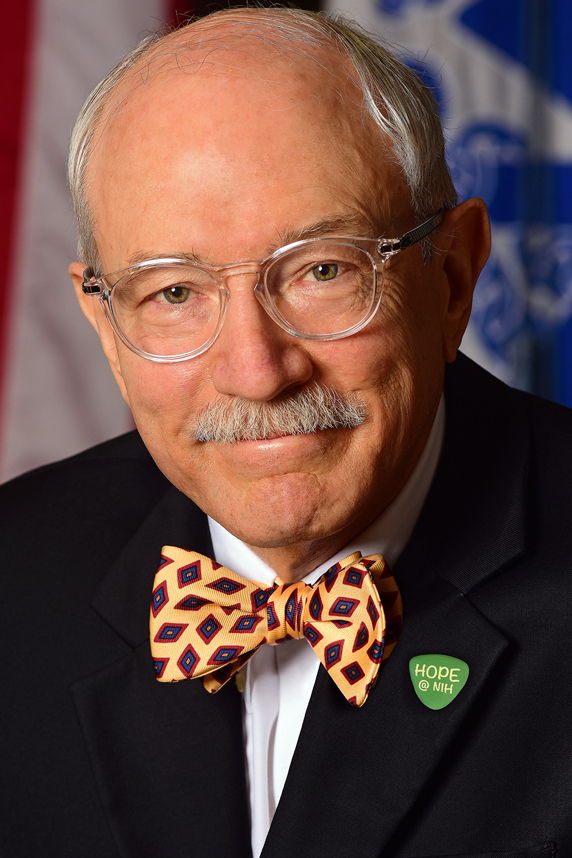 “We also hope that education will help to both eliminate environmental health disparities and positively address environmental justice,” Woychik said. (Photo courtesy of Steve McCaw / NIEHS)
“We also hope that education will help to both eliminate environmental health disparities and positively address environmental justice,” Woychik said. (Photo courtesy of Steve McCaw / NIEHS)In addition, two Spanish language sessions — chaired by Gabriela Livas Stein, Ph.D., a psychology professor at University of North Carolina at Greensboro — were offered for the Latina community. She shared strategies for self-care and discussed the role of neighborhoods in shaping health.
Health disparities are pervasive
NIEHS and National Toxicology Program Director Rick Woychik, Ph.D., lauded the efforts of the WHA planning and steering committees for tackling important topics.
“Health disparities are more pervasive than we previously recognized,” he said. “We have a lot of work to do to bring equity in environmental health and resiliency to communities of color.”
Educational health and wellness sessions addressed diabetes, cancer, Alzheimer’s disease, COVID-19, behavioral health, healthy nutrition, and mindfulness. Environmental health sessions covered the maternal mortality crisis, endocrine disruptors and infertility, environmental justice, housing disparities, and disaster preparedness.
Our homes, our health
U.S. Department of Housing and Urban Development (HUD) Secretary Marcia L. Fudge delivered pre-recorded remarks on housing discrimination and health. Fudge highlighted the importance of safe, affordable housing for health.
 “Housing is not only a roof over one’s head. It is the platform and foundation for every other life outcome. Housing is foundational to health,” Fudge said. (Photo courtesy of Marcia Fudge)
“Housing is not only a roof over one’s head. It is the platform and foundation for every other life outcome. Housing is foundational to health,” Fudge said. (Photo courtesy of Marcia Fudge)“Where you live affects your access to jobs, food, education, and health care, and whether you are exposed to environmental pollutants or lead,” Fudge said. “It also determines your outcomes in pregnancy and birth, infant mortality, and life expectancy.”
Fudge spoke about climate change and its impact on health. She noted that underserved communities — especially those who live in flood zones near industrial sites, brownfields, and waste dumps — are often disproportionately affected by climate change. Fudge added that such individuals are exposed to health risks, environmental hazards, and substandard housing.
“We work with the Department of Health and Human Services to integrate health with housing [because we] recognize housing’s role as a social determinant of health,” she said.
Fudge shared that the gap between the rates of Black and white home ownership is greater now than when the Fair Housing Act was passed 54 years ago. She indicated that HUD is working to tackle the root causes of discrimination in homeownership because owning a home is a great source of generational wealth.
Following Fudge’s remarks, a panel of experts discussed housing issues in North Carolina and provided resources for housing insecurity and low-quality housing.
Maternal mortality on the rise
 “We are doing worse than we were 20 years ago,” Murdock said about maternal mortality and reproductive health. “We know North Carolina can do better.” (Photo courtesy of Natalie Murdock)
“We are doing worse than we were 20 years ago,” Murdock said about maternal mortality and reproductive health. “We know North Carolina can do better.” (Photo courtesy of Natalie Murdock)North Carolina State Senator Natalie Murdock noted the U.S. has the highest maternal mortality rate in the developed world.
“The U.S. is one of only 13 countries where maternal mortality is on the rise,” she said. “North Carolina ranks 30th among U.S. states. Racial disparities are driving this health crisis, with Black women disproportionately affected.”
Janine Clayton, M.D., director of the Office of Research on Women’s Health at the National Institutes of Health, noted that in 2020, more than 50,000 women experienced severe, sometimes life-threatening complications during childbirth. She noted that Black women have a 2.9% higher death rate from childbirth than white women.
“Maternal mortality rates in the U.S. are at a crisis level and are continuing to rise,” Clayton said. “In 2020, 861 women died, and 60% of those deaths were preventable.”
Understanding maternal mortality
Insufficient minority representation in clinical research is an important factor in understanding the maternal mortality crisis in America, Clayton added.
“I encourage people of color to participate in studies if they have an opportunity to do so, even if it’s just a survey,” she said. “Participation might help overcome implicit bias underlying the disparities in minority health outcomes.”
 Clayton noted pregnancy correlates with increased risk of homicide, and pregnant Black women have up to nearly a threefold higher risk of dying by homicide than those who are not pregnant. (Photo courtesy of Janine Clayton)
Clayton noted pregnancy correlates with increased risk of homicide, and pregnant Black women have up to nearly a threefold higher risk of dying by homicide than those who are not pregnant. (Photo courtesy of Janine Clayton)Maria Small, M.D., from Duke University School of Medicine, chaired the N.C. Department of Health and Human Services Maternal Mortality Review Committee that recently released the North Carolina Maternal Mortality Review Report. According to Small, there has been a significant shift in recent years in attitudes about health inequity.
“We’ve talked about health inequities for a long time, but it wasn’t until recently that we had some very strong advocates for change,” she said.
The WHA event was sponsored by NIEHS, the Durham Alumnae Chapter of Delta Sigma Theta Sorority Inc., Durham Alumnae Delta House Inc., and the North Carolina Central University Department of Public Health Education.
(John Yewell is a contract writer for the NIEHS Office of Communications and Public Liaison.)
Source link
factor.niehs.nih.gov


