1. Introduction
In today’s society, there is an increasing recognition that diversity, equity, inclusion, and accessibility (EDIA) are important issues. While it has always been important to embrace diversity, recent social movements have brought global awareness to these issues. Embracing workplace diversity offers numerous advantages. Diverse teams are often more innovative, creative, productive, and smarter [
1,
2]. Equitable representation in medicine and within medical education has been shown to have a multitude of benefits. Embracing gender diversity specifically has been shown to improve care of marginalized populations, strengthen patient–physician communication, foster inclusive environments and diverse recruitment, as well as enhance learning in medical schools [
3,
4,
5,
6,
7,
8,
9]. The benefits of gender equity have also been demonstrated in other fields such as business [
10], and specific calls to action for equity have created instrumental change in disciplines such as law [
11] and media relations [
12].
In the operating room, increased anesthesia–surgery team sex diversity has been shown to be associated with better post-operative outcomes [
13]. Female representation within surgical specialties in American and Canadian residency programs has increased in recent years, but persistent gender gaps still remain [
14,
15,
16,
17,
18,
19,
20]. In Canada, studies have been carried out on gender representation within otolaryngology [
18,
19]. Both studies found increases in female representation over their respective time periods [
18,
19]. One study compared otolaryngology to other surgical and non-surgical specialties [
19]. Although improvements in female representation were noted in all specialties, absolute representation was found to vary significantly, suggesting that gender gaps remain in certain specialties [
19]. In the United States, studies have been carried out within several surgical specialties [
14,
15,
16,
17]. Increases in female representation have been noted in multiple studies [
14,
15,
16]; however, degree of improvement as well as absolute female representation varies depending on the specialty, again suggesting that gender gaps remain in certain areas [
15,
16].
With recent studies showing improved short- [
21] and long-term [
22] post-operative outcomes for patients treated by female surgeons, in addition to the aforementioned benefits of gender-diverse teams, the importance of increasing female representation in surgery is clear. As we implement actionable changes to address gender equity within surgical training, it is necessary to evaluate trends of current disparities. This study aims to identify the current and recent past state of gender diversity of trainees entering Canadian surgical residency programs by specialty.
2. Materials and Methods
Data were sourced from the Canadian Post-M.D. Education Registry (CAPER) and the Canadian Resident Matching Service (CaRMs) [
23,
24]. Each year, CAPER produces an annual summary of postgraduate medical trainee characteristics, including information such as trainee specialty, age, training location, gender, and place of graduation [
23]. CaRMs compiles detailed annual statistics on the residency match, including number of applicants and matched individuals, as well as demographic information [
24]. For both these services, data are available upon request [
23,
24].
CAPER data were publicly available for PGY-1 trainees in all surgical specialties by gender (male/female) for the academic years 2012–2013 to 2021–2022. Surgical specialties were defined as cardiac surgery, general surgery, obstetrics/gynecology, ophthalmology, otolaryngology head and neck surgery, orthopedic surgery, plastic surgery, urology, and vascular surgery. These data include trainees who are Canadian citizens or permanent residents at all 17 Canadian academic centers with surgical residency programs.
CaRMs provided data of total applicants and matched applicants for Canadian Medical Graduates (CMGs) by gender for all aforementioned surgical specialties in the match years 2013 (when gender data collection began) to 2022. These data exclude any applicants who did not disclose their gender or identified as “X”. The match rate was calculated using the number of matched applicants by gender divided by the number of applicants of the same gender. The match rate reflects the percentage of applicants of a certain gender who matched.
Descriptive and chi-square statistics were performed. Our threshold for statistical significance was p < 0.05. Ethical approval was waived by the University of Alberta Research Ethics Office as the study used only publicly available data.
3. Results
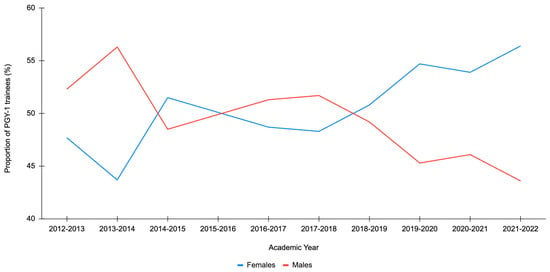
For the academic years 2012–2013 to 2021–2022, there were 4011 PGY-1 surgical residents across all Canadian academic centers (
Table S1). Of this cohort, 2023 (50.4%) were female and 1988 (49.6%) were male (
Table S1). In certain years, there were more female residents than male residents, while in other years, it was the opposite (
Figure 1). The 2021–2022 academic year showed the highest proportion of PGY-1 female trainees at 56.4% and the lowest proportion of male trainees at 43.6% (
Figure 1). Conversely, the 2013–2014 academic year showed the highest proportion of PGY-1 male trainees at 56.3% and the lowest proportion of female trainees at 43.7% (
Figure 1). Although the distribution has varied by year, when comparing the proportions between genders, there was no statistically significant difference in any year (
p > 0.20).
Additionally, the gender distribution of PGY-1 surgical residents is not equitable amongst all specialties (
Table S1). The surgical specialties with the most female representation over this time period were obstetrics/gynecology (82.1–91.9%), general surgery (40.2–70.7%), and plastic surgery (33.3–54.2%) (
Table S1). The surgical specialties with the least female representation over this time period were neurosurgery (18.8–35.3%), urology (11.8–42.0%), and orthopedic surgery (17.5–38.5%) (
Table S1).
Amongst female applicants, the number of applicants was greatest in 2022 at 378, while it was the lowest in 2015 at 307 (
Figure 2). Amongst male applicants, the number of applicants was greatest in 2013 at 339, while it was the lowest in 2020 at 266 (
Figure 2). Comparing 2013 to 2022, the number of female applicants to surgical programs has increased, while the number of male applicants has decreased (
Figure 2). Female applicants outnumber male applicants each year starting in 2014 (
Figure 2). Although female applicants outnumbered male applicants in all years (except 2013), the difference in proportions was not statistically significant for any of the first six years (
p > 0.14). There was a statistically significant difference between genders for each of the last four years (2019, 2020, 2021, and 2022) (
p < 0.003).
The number of matched female applicants was greatest in 2022 at 210, while it was lowest in 2017 at 174 (
Figure 3). The number of matched male applicants was greatest in 2013 at 223, while it was lowest in 2020 at 154 (
Figure 3). Comparing 2013 to 2022, the number of matched female applicants to surgical programs has increased, while the number of matched male applicants has decreased (
Figure 3). The number of matched female applicants was greater than the number of matched male applicants each year except 2013, 2016, and 2017 (
Figure 3). However, the difference in proportions was not statistically significant for any of the first eight years (
p > 0.05). For the last two years, there was a statistically significant difference between genders (2021 and 2022) (
p < 0.02).
Amongst female applicants, the match rate to surgical programs has varied year by year, with the highest being 63.9% in 2014 and the lowest in 2018 at 48.8% (
Figure 4). Amongst male applicants to surgical programs, the highest match rate was 67.6% in 2015 and the lowest match rate was 53.3% in 2018 (
Figure 4). In all years except 2014, 2020, and 2021, the female match rate was lower than the male match rate, although there was not a statistically significant difference in any year (
p > 0.32). The greatest gap in match rate to a surgical discipline was in 2017, where 52.6% of female applicants matched compared to 63.4% of male applicants. In the most recent application cycle in 2022, 378 (56.8%) applicants to all surgical disciplines were female and the match rates by gender were similar for both female (55.6%) and male (56.8%) applicants.
4. Discussion
Starting in the 2017–2018 academic year, the proportion of female PGY-1 surgical residents has generally been trending upwards across all specialties; the 2021–2022 academic year marked the highest proportion of female PGY-1 surgical residents in Canadian training programs in the last decade. Furthermore, certain specialties show great representation of female residents, including obstetrics/gynecology, general surgery, and plastic surgery. Additionally, the 2022 residency match had the highest number of female applicants to all surgical disciplines. From 2019 to 2022, there was a statistically significant difference in the number of applicants, with more female than male applicants. The 2022 residency match also had the highest number of matched female applicants, and in both 2021 and 2022, there was a statistically significant difference in the number of matched applicants by gender. It is encouraging to see that in the years with higher numbers of female applicants, this was reflected in match rates, suggesting equal consideration of both genders. As the number of female applicants increases, it is fitting that more would match; ultimately, one could argue that despite the absolute number of applicants, the match rates between genders should be the same. In our study, no statistically significant difference was observed in match rates between genders in any year, which is quite encouraging. Overall, these are promising trends that reflect increased surgical interest amongst female trainees and improving gender equity in surgical training.
For the past five years, the proportion of female PGY-1 surgical residents in Canada has been steadily increasing. In 2021–2022, 56.4% of PGY-1 surgical residents in Canada were female. Comparatively, in 2016, 50.9% of the general Canadian population were female [
25]. Hence, female representation among PGY-1 surgical residents in Canada is similar to demographic proportions, which is quite encouraging to reflect the populations we serve.
While the number of female trainees in general surgery and obstetrics/gynecology programs match and even exceed Canadian demographic proportions [
25], this is not true for most other surgical specialties. For example, neurosurgery has remained relatively constant with only a 16.5% variation in the proportion of female trainees in the last ten years. Other specialties such as orthopedic surgery, urology, and cardiac surgery also do not reflect overall trends and continue to demonstrate the lowest proportion of female trainees. Similar disparities exist in American programs, as a study of cardiothoracic training programs found that 24% of trainees were female in 2019 [
14]. Additionally, other studies have found that in American orthopedic training programs, 16% of trainees were female in 2020 [
15], and 18% of neurosurgery trainees were female in 2017 [
17].
When discussing gender equity, it is also important to consider the nature of the specialty. In our study, the majority of urology trainees were male, and most obstetrics/gynecology trainees were female. There may be an argument to be made that these numbers may better reflect the patient population of the respective specialties, and that patient preference is a complex factor to consider in the discussion of gender equity. However, the results regarding preference for surgeon gender for urology and obstetrics/gynecology are actually quite heterogenous, with some studies showing that patients have a strong preference in the gender of their surgeon [
26,
27,
28,
29,
30], whereas other studies find no significant preference amongst both male and female patients [
31,
32].
Evaluating the reasons for why specialties such as neurosurgery, urology, and orthopedic surgery have been slow to make progress is complex and likely rooted in structural and systemic factors. Studies examining factors influencing female medical students to pursue surgical careers identify mentorship, specialty exposure, nature of the surgical field, gender discrimination, and personal factors to be significant predictors of surgical career choice [
33,
34]. Additionally, dispelling a common misconception, female trainees have not been found to be more likely than male trainees to identify lifestyle and family priorities as important factors [
33]. This reflects a change in values and attitudes of all trainees compared to previous generations. These factors have also been consistent over the last decade, with research opportunities emerging as an additional motivator for trainees in recent years [
35]. Some of these listed factors may not be modifiable, such as nature of surgical field (e.g., length of training in neurosurgery being six years compared to five years of all other surgical specialties) and personal factors. However, the remaining factors present avenues to continue to improve representation of female trainees.
We do not have to reinvent the wheel when thinking of early career interventions at the medical student stage, and rather we should look to specialties such as obstetrics/gynecology, general surgery, and plastic surgery to identify what changes have been made and what is currently being done to achieve progress in gender equity amongst incoming residents. A multifaceted approach, with a primary focus on enhancing the visibility of underrepresented trainees, would likely be effective in promoting diverse trainee recruitment [
36,
37]. This may include mentorship/outreach programs, inclusive residency program selection criteria and evaluation, program diversity training [
36], and increased academic opportunities for underrepresented trainees [
37]. As general surgery and obstetrics/gynecology are mandatory rotations for medical students at most Canadian institutions, the combination of increased exposure, interaction with female staff surgeons, and opportunities for mentorship may play a role in pursuing these specialties for female applicants. On the other hand, male trainees have consistently remained underrepresented in obstetrics/gynecology, with only a 9.8% variation over the ten-year period. This may be due to lack of opportunity for mentorship within the specialty by male staff surgeons.
As we see progress in gender equity in surgery at the medical student and resident level, it is important to look ahead and consider attrition and retention of female surgeons as staff. The Canadian Institute for Health Information released a report that showed only 34% of practicing surgeons were female compared with 45% of all physicians in Canada in 2022 [
38]. The Canadian Medical Association specialty profile demonstrates there is a poor representation of female staff surgeons (
Figure 5) [
39]. For example, in 2019, 28% of general surgeons in Canada were female compared to 43.9% female PGY-1 general surgery residents in 2012 [
40]. Given the seven-year period between 2012 and 2019, most of these residents would have completed their five-year program, and if applicable, up to two years of fellowship. Hence, one would expect these two percentages to be more closely aligned. A retrospective review examining attrition over the past decade found that the attrition rate for female surgical trainees was 12.4% and decreasing overall; however, female residents were twice as likely to leave training compared to their male counterparts [
41].
Similar to trainees entering residency, there are both modifiable and non-modifiable factors shown to impact female surgeons in career advancement. A survey of general surgery residents in Canada showed that residents who self-identified as women or a visible minority were less likely to report they had a collegial relationship with staff, feel like they fit in with their training programs, and feel valued at work [
42]. An inclusive culture is clearly one of the factors associated with maintaining the diversity of female residents through their training. In addition, factors such as gender discrimination, lack of mentorship, and pay inequity act as barriers to advancement in surgical careers [
43,
44,
45]. An even larger disparity exists when examining the proportion of female surgeons in leadership positions [
40,
46]. In 2021, only 10% of division heads in Canadian surgical programs were female, and just 11% of surgical department chairs [
40]. Fewer practicing staff surgeons and even fewer female surgeons in leadership raise continued concern for the “leaky pipeline” in which female surgeons decrease by proportion at each level of ascending leadership or prestige. Increased administrational and academic opportunities are needed for female surgeons, as well as surgeons from underrepresented populations. Further steps to ensure the structures, policies, and practices of surgical residency and faculty programs reflect inclusive cultures, supportive training environments, and institutional structures that actively combat loss of female participation in surgical specialties will be vital in the next decade.
Increasing gender diversity would be beneficial in terms of organizational performance, patient care, inclusivity, diverse recruitment, and education. Within research teams, increased gender diversity fosters innovation and creativity, builds smarter teams, and effectively utilizes each team member’s expertise, opening doors to new advancements [
1]. Furthermore, heterogeneity in teams has been shown to enhance group performance and productivity by incorporating a wide range of perspectives [
2]. In medicine, embracing gender, racial, sexual, and socioeconomic diversity has been shown to result in more effective care of systematically marginalized patient populations [
3,
4]. Additionally, when patients and physicians share the same race or language, it can lead to enhanced communication within the patient–physician relationship, ultimately improving health outcomes [
5]. Diverse workforces in medicine that represent the patients they serve create more inclusive environments that acknowledge and understand their patient’s worldviews [
6]. Within medical education, increased women surgical faculty representation is positively associated with women medical students choosing surgery as a career [
7]. Additionally, diversity among professors and students has been shown to enhance learning in medical schools [
8,
9]. Furthermore, benefits of gender equity are not isolated to scientific disciplines and have been demonstrated in several other fields such as business, law, and media relations [
10,
11,
12].
Studies have also shown greater sex diversity within the operative team, as well as female-led surgeries, to be associated with improved post-operative outcomes [
13,
21,
22]. A study carried out within Canadian hospitals found greater sex diversity within anesthesia–surgery teams to be associated with a lower likelihood of major morbidity within 90 days [
13]. Furthermore, Canadian studies have shown that patients treated by female surgeons experience lower mortality and complication rates at 30 days, 90 days, and one year [
21,
22].
Similar to our study, Bondok and colleagues utilized CaRMs to carry out a retrospective study on gender trends within Canadian surgical residency, with congruent results [
20]. However, our study utilized data from both CaRMs as well as CAPER and hence provides additional context by specialty. A limitation of acquiring data from CaRMs is that if there are fewer than five matched residents for a given year and specialty, the exact number is not given to prevent identification of the physicians in question, which can limit the ability to identify trends at the specialty level. To overcome this limitation, in our study, CAPER was used to identify trends at the specialty level by year. Therefore, rather than comparing trends every five years, our study was able to make comparisons at the specialty level in each individual year (
Table S1), which ultimately allowed for a more nuanced analysis.
A limitation of this study is that gender data to both CaRMs and CAPER are self-reported and do not capture applicants who preferred not to disclose that information or identify as non-binary. These data are not reported by CAPER and were only very recently recorded by CaRMS. Additionally, we were unable to correlate other intersectional identity components of applicants such as race, sexuality, or socioeconomic status with gender as these data are not publicly available. With the recent implementation of the CaRMS self-identification questionnaire and awareness of intersectional identity in other surveys, we look forward to the availability of these data to further add to the discussion of equitable representation in surgery.