3. Discussion
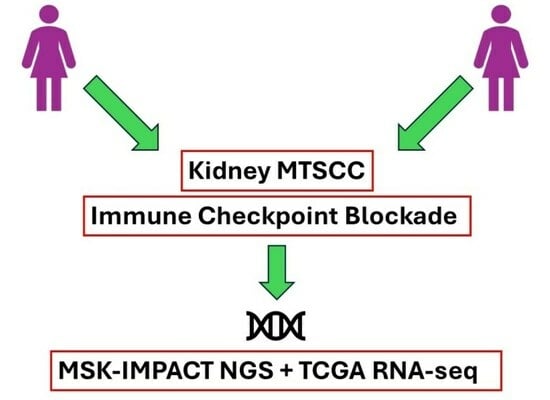
We describe two patients with high-grade, metastatic MTSCC treated with first-line ipilimumab plus nivolumab who sustained clinical benefit. The first patient underwent serial metastatectomy for oligo-progressive disease with a continued treatment-free interval; in contrast, the second patient, who also developed oligo-progressive disease after combination ICB therapy was switched to second-line combination treatment with VEGFR TKI and ICB on a clinical trial that was subsequently discontinued due to treatment-related toxicities. The exhibited prolonged clinical benefit, though, was thought to be conferred by initial first-line ipilimumab plus nivolumab therapy. These cases support prior reports demonstrating significant clinical benefit in MTSCC tumors treated with combination dual ICB therapy and support consideration and prospective study of this treatment regimen in this extremely rare RCC tumor subtype.
Several prospective and retrospective reports have highlighted the variability of the efficacy of ICB-based therapy in non-clear cell RCC tumors. Combination ICB/VEGF therapy is associated with the highest overall response rates, with treatment efficacy observed with regimens including cabozantinib plus nivolumab [
9] and lenvatinib plus pembrolizumab [
10]. Notably, both phase II trials enrolled patients with non-clear cell RCC histologies including papillary, unclassified, translocation-associated and chromophobe subtypes but did not include MTSCC histology. In the CheckMate-920 study, other non-clear cell RCC histologies also were allowed like collecting duct and renal medullary carcinoma but did not include MTSCC patients in their cohorts and thus the overall experience with dual ICB/ICB therapy for non-clear cell histologies has been limited [
11,
12]. Recent results from SUNNIFORECAST, the first prospective randomized trial of ipilimumab + nivolumab in non-clear cell RCC has gained significant attention [
13]. This trial included 178 non-clear cell RCC patients, the majority of whom had papillary RCC (57.6%), and chromophobe RCC (19.4%). Across the whole population, patients with tumors harboring PD-L1 > 1% had a favorable response to the ipilimumab + nivolumab (HR 0.56, 95% CI: 0.33–0.95) preliminary suggesting this as a biomarker in non-clear cell RCC histologies. While the trial included 50 patients with other rare non-clear cell RCC subtypes, it is not known at this time whether any patients had MTSCC [
13].
Use of either VEGFR TKI or ICB therapy for MTSCC has shown mixed outcomes in case reports and case series. In a retrospective review of MTSCC patients, variable benefit was seen with VEGFR TKIs including sunitinib, pazopanib, cabozantinib and other VEGF inhibitors such as bevacizumab. Most of these reports, though, include patients with MTSCC and high-grade/sarcomatoid disease and this again may be related to the inherent aggressive nature of such cases. For patients treated with ICB therapy, experience has additionally been variable. In a series of 41 patients with non-clear cell RCC treated with nivolumab, one patient with metastatic MTSCC had disease progression [
14]. In another report, a patient who experienced progression on VEGFR TKI and subsequently developed a complete response to single agent nivolumab [
15]. Fuchizawa et al. reported a case of metastatic PD-L1+, MSS, TMB-low MTSCC with an
FBXW7 nonsense mutation with metastases to the bone treated with ipilimumab plus nivolumab as first-line therapy. After four cycles of combination ICB therapy, the patient received nine cycles of nivolumab followed by delayed cytoreductive radical nephrectomy, with resumption of nivolumab without progressive disease at 15 months, at which point therapy was terminated given no evidence of disease [
6]. Chahoud et al. reported on one patient with MTSCC who had stable disease and progression-free survival of 7.4 months on nivolumab [
16].
In the context of biomarkers associated with clinical benefit to ICB therapy, several unique features were apparent in our two patients. In the first case, the patient was found to have mismatch repair (MMR) deficiency in the original tumor by molecular profiling. While this patient was included in a larger series of MTSCC patients reported from our institution [
2], we present here treatment response data which were not reported previously. MMR deficiency or microsatellite instability (MSI) is not a feature commonly found in RCC tumors but alterations in DNA damage response (DDR) pathways have previously been shown to be associated with ICB response in ccRCC [
17]. Our report also included MTSCC tumor with sarcomatoid and rhabdoid features, which often in ccRCC display a highly inflamed subtype characterized by immune activation and PD-L1 expression [
18]. It is unknown though whether rhabdoid/sarcomatoid MTSCC tumors display similar molecular findings. Nevertheless, exploratory analyses from CheckMate-214, the phase III registration study of ipilimumab plus nivolumab, showed that ipilimumab plus nivolumab had high overall response and complete response rates in ccRCC with sarcomatoid features [
19].
MTSCC tumors are characterized by recurrent chromosomal changes [
7]. In contrast to pRCC patients within TCGA and other studies, MTSCC tumors show multiple chromosomal gains including nearly universal gains of chromosomes 7 and 17 and less frequent gains of chromosomes 2, 3, 12, 16 and 20 [
20,
21]. These findings corroborate results by Mehra et al. [
7] and support the notion that MTSCC harbor distinct and characteristic chromosomal copy number alterations. Other groups have shown losses of chromosomes 1, 2, 4 through 10, 12 through 15, 17, 20, 22 and X in MTSCC while lacking in trisomy 7 or 17 [
1,
4,
5,
7,
21,
22,
23]. Ged et al. identified a loss of heterozygosity (LOH) of chromosomes 1, 15 and 22 in 100% of cases, 6, 9 and 13 in 80% of cases and 14 in 60% of cases [
2]. Given the overall challenge in diagnosing MTSCC tumor types, molecular analysis particularly beyond platform testing to identify copy number alterations may be helpful in discerning profiles associated with MTSCC.
An analysis of the pRCC cohort within the TCGA (KIRP) demonstrated that five tumors molecularly resemble an MTSCC phenotype rather than KIRP [
7]. We performed immune deconvolution analysis of these MTSCC-like tumors compared to KIRP and discovered significant upregulation of PD-L1 and decreased expression of antigen presentation machinery (APM1, APM2) (
Figure 2). This finding is concordant with the prior case report demonstrating high PD-L1 expression by IHC [
6]. Interestingly, PD-L1 expression has been shown to be higher in the spindle components relative to tubular components in MTSCC. Also, the expression of PD-L1 is reportedly higher at the surface of sarcomatoid RCC cells compared to non-sarcomatoid RCC cells, regardless of the parent histology or non-sarcomatoid RCC tumor grade [
24,
25,
26]. These findings, in conjunction with the published clinical data, support the observed activity of ICB therapy in PD-L1+ high-grade MTSCC tumors.
Prior efforts profiling MTSCC tumors have shown that almost uniformly all MTSCC patients harbor dysregulation of the Hippo signaling pathway, including alterations in
NF2, a feature also found in a subset of highly aggressive unclassified RCC tumors [
27], as well as alterations in other Hippo-related genes. Prior IHC analysis has shown nuclear YAP1 (90%) and increased YAP protein levels (68%) in MTSCC tumors [
7]. These data suggest that Hippo pathway dysregulation may be a seminal event in the pathogenesis of MTSCC and may have diagnostic and therapeutic implications for this malignancy. Targeting the Hippo pathway and YAP/TAZ has been an active interest in conventional RCC tumors given implications of hypoxia inducible factor pathway [
28], and these data additionally suggest that particularly non-clear cell RCC like MTSCC may similarly be sensitive to oral Tead1 inhibitors [
29], which in turn could be combined with PD-1/PD-L1 agents.