1. Introduction
The three leading causes of human death globally are cardiovascular disease, stroke, and chronic obstructive pulmonary disease [
1]. In 2021, cardiovascular diseases were the leading cause of mortality worldwide [
1], with myocardial infarction (MI) responsible for most of the 17.9 million cardiovascular-related deaths reported in 2019 [
2,
3]. Historically, the incidence of MI was believed to increase with age due to severe myocardial damage [
4]. However, chronic diseases, such as hypertension, stroke, and hyperlipidemia, have an earlier onset, making MI increasingly common among middle-aged adults. In the United States, the hospitalization rate of middle-aged adults for MI increased from 27% in 1999 to 32% in 2014, with the one-year post-cardiac arrest mortality rate reaching 10% [
5]. Approximately 47% of patients with MI in China are middle-aged adults [
3], and in South Korea, the incidence rate of cardiac arrest among middle-aged adults is as high as 74.5% [
6,
7,
8].
Cardiac arrest is a complex condition where structural or functional impairments in the heart make normal blood circulation impossible, halting blood flow to the brain and vital organs [
9]. Most out-of-hospital cardiac arrests occur in community settings and have high mortality rates, posing a significant public health burden [
10]. The Korea Disease Control and Prevention Agency recommends that all citizens learn and perform cardiopulmonary resuscitation (CPR), with training provided to healthcare professionals and the public by the Korean Association of Cardiopulmonary Resuscitation. Factors affecting CPR performance, such as knowledge, confidence, teamwork, skills, and self-efficacy, have been studied, but most research is limited to in-hospital cardiac arrests or focuses on medical professionals [
11,
12,
13].
The effective performance of CPR by the first witness of a cardiac arrest is the most crucial factor in increasing patient survival rates. Bystander CPR improves survival rates by 10% per minute [
14]. Middle-aged adults are likely to encounter emergencies such as cardiac arrest at home and work, and anyone in the community can become a bystander, necessitating accurate CPR skills. Enhancing CPR performance capabilities in this population can significantly improve life-saving effectiveness and emergency response abilities. Additionally, as role models for younger generations, middle-aged adults can emphasize the importance of CPR knowledge and skills, contributing to improved emergency response capabilities across society. Thus, strengthening the CPR performance abilities of middle-aged adults provides critical benefits both individually and socially.
Despite the increasing incidence of MI among middle-aged adults, research analyzing their recognition of early MI symptoms and CPR training experiences is lacking. Some studies have examined the effects of external interventions, including telephone dispatcher-assisted CPR, on bystander CPR performance [
15,
16]; however, more research is needed on factors related to the bystander initiation of CPR in out-of-hospital cardiac arrest situations.
This study aimed to utilize data from the 2022 Korea Community Health Survey [
17] to assess the level of recognition of early MI symptoms among middle-aged adults and identify factors affecting CPR performance based on CPR training experiences. The findings are intended to provide foundational data for developing CPR training programs for middle-aged adults.
4. Discussion
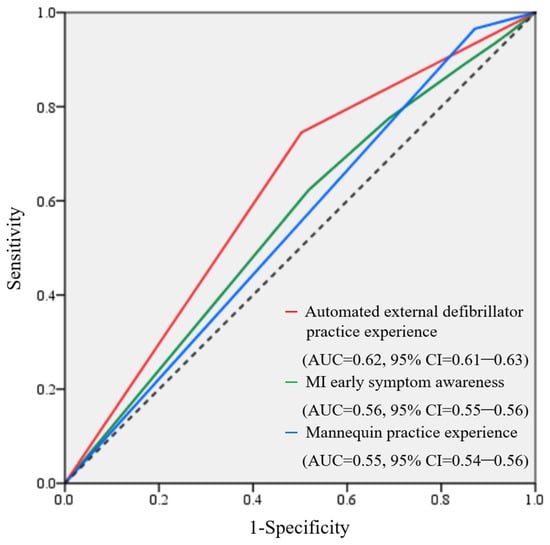
With conditions leading to cardiac arrest becoming increasingly prevalent, including MI, hypertension, and stroke, enhancing the ability of the general public to perform CPR can significantly reduce mortality rates. The effective resuscitation of patients undergoing cardiac arrest involves a continuous sequence of these five links in the survival chain: (1) the recognition of cardiac arrest and calling for help, (2) bystander CPR, (3) defibrillation, (4) advanced life support, and (5) post-resuscitation care. This study was conducted to identify factors affecting the CPR performance ability of middle-aged adults, providing a basis for developing programs to strengthen the survival chain. Our main findings indicate that with each incremental increase in the recognition of MI early symptoms, CPR performance ability improved by approximately 9–22%. In contrast, the lack of experience with mannequin training resulted in a 51–79% reduction in CPR performance ability, and the absence of AED training experience led to a 46–77% decrease in performance ability.
Only 15.5% of the 99,945 middle-aged adults could perform CPR accurately. Although direct comparisons are challenging due to limited studies on middle-aged adults’ CPR performance, this figure is lower compared to those reported in Japan (40.2%), Singapore (24.3%), Malaysia (22.6%), and Thailand (15.8%) [
19]. The immediate initiation of CPR by the first bystander is crucial for improving survival rates [
14,
20]; however, the general CPR performance rate among all age groups in Korea was only 29.2% in 2022 [
21]. This suggests the need to address barriers to CPR training and participation, considering factors such as age, understanding, infrastructure, and educational information, and to promote tailored educational programs.
Over 60% of the study participants were aware of the five early symptoms of MI. However, those who could not perform CPR accurately had lower awareness rates for each symptom than those who could perform CPR accurately. Particularly, recognition rates for pain in the jaw, neck, and back, as well as pain in the arms and shoulders, as MI early symptoms were lower. This is consistent with the results of a systematic review of MI early symptom awareness among the public in 35 countries, which found that the recognition of chest pain was the highest, whereas the awareness of jaw, neck, and back pain was lower [
22]. The knowledge of MI early symptoms may vary by age, race, and socioeconomic status [
23], and one of the key goals of CPR education is to enable the public to quickly recognize and intervene in cardiac arrest situations to minimize delays and save lives, as incomplete awareness can lead to the delayed or missed initiation of CPR [
24,
25]. As the public may find it challenging to connect pain in the jaw, neck, back, arms, and shoulders with early MI symptoms, future CPR education programs should emphasize this knowledge to strengthen the first link in the survival chain. Furthermore, understanding the reasons for the lower recognition rates for certain symptoms could inform targeted interventions. For instance, tailored education strategies that focus on the importance of recognizing atypical symptoms, such as pain in the jaw and shoulders, could improve overall awareness and preparedness for MI.
The association between CPR training experience and CPR performance ability is well-established in the literature [
24,
26,
27]. Moreover, practical training with equipment has been reported to markedly enhance CPR skills compared to lecture-based training without hands-on practice [
28]. Trained individuals are highly likely to start CPR faster, report to emergency medical services, and use an AED three times more frequently [
26]. Practical training experiences thus positively influence the first three stages of the survival chain, improving survival rates. However, CPR training coverage varies globally, ranging from 3–79%, and the proportion of the public receiving training within the past two years remains relatively low [
27]. Regular opportunities for practical training should be provided, and efforts should be made to streamline training programs and enhance accessibility. For instance, Japan has incorporated CPR training into school curricula and driver’s license requirements [
19], and Korea is producing and distributing educational videos to facilitate easy learning of CPR [
21]. Nonetheless, training for AED use and the recognition of cardiac arrest situations are lacking. Therefore, improvements in programs through diverse audiovisual materials and self-study resources are necessary. Although scenario-based training and feedback devices positively impact CPR skill acquisition and performance [
29,
30], studies have found no relationship with patient outcomes [
31,
32]. Thus, further research is needed to develop and validate programs aimed at enhancing accurate CPR performance in middle-aged adults.
This study had some limitations. First, it was a secondary data analysis focusing solely on middle-aged adults in Korea, which limits the variability of variables and generalizability of the results. Second, the difference in sample sizes between the groups based on their CPR performance ability may have influenced the results, requiring cautious interpretation. The larger group size could have led to more statistically significant findings, potentially skewing the overall interpretation. Nevertheless, this study contributes to raising societal awareness and emphasizing the importance of the knowledge of MI early symptoms and CPR practical training experience by identifying factors affecting the CPR performance ability of middle-aged adults. This, in turn, can enhance emergency response capabilities and strengthen the overall safety net of society.
The literature clearly strengthens the association between the early recognition of MI symptoms and the success of life-saving efforts, such as CPR. Our findings elucidate previously unknown associations between the ability of middle-aged adults to recognize the early symptoms of MI, their CPR and AED training history, and their self-reported ability to complete CPR in emergencies successfully. Enhancing the recognition of early MI symptoms and providing hands-on CPR training is vital for improving CPR performance among middle-aged adults and enhancing the overall social safety net.