Antiretroviral therapy (ART) has significantly reduced AIDS-related morbidity and mortality by slowing down HIV replication to the point where the viral load (VL) in the peripheral blood is undetectable [1,2]. To date, triple therapy (TT) regimens remain the “gold standard” for HIV treatment in resource-limited settings, whereas dual therapies (DT) are among the first choices in the majority of Western guidelines. With this ART strategy, the number of new HIV infections has fallen by more than 60% since the peak in 1995–1997 [1]. However, there are still 39 million people living with HIV (PLHIV) globally (with Sub-Saharan Africa accounting for more than 70%), and 1.3 million people newly infected in 2022 [1]. In 2022, in Cameroon, 480,228 people were living with HIV, with 9898 new HIV infections and 10,198 people dying of an AIDS-related illness [3]. Despite efforts to move towards remission or even lasting eradication of HIV, lifelong ART regimens appear to be the only option for patients to restore and maintain good health [4]. However, in the context of lifelong ART, there is a growing need for treatment simplification strategies to minimize the cumulative toxicity of drug exposure [5], while also improving patients’ adherence to their ART. For more than two decades, in low- and middle-income countries (LMICs) like Cameroon, the backbone for all ART-regimen lines (first, second and third) has been the combination of two nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs) such as tenofovir disoproxil fumarate (TDF), lamivudine (3TC), zidovudine (AZT) or abacavir (ABC) [6]. Of note, some of these NRTIs have been associated with bone, renal and metabolic toxicities that are superimposed on the comorbidities associated with aging [7,8,9] and can lead to significant problems, including long-term toxicity and adherence [10,11]. Therefore, managing PLWH with multimorbidity and polypharmacy remains a significant challenge for clinicians and requires the implementation of new ART strategies like DT. DT combining integrase inhibitors and non-NRTIs (NNRTIs) represents a promising regimen in aging HIV-infected individuals with long exposure to nucleoside analogues and protease inhibitors (PIs) [5]. Etravirine (ETR), rilpivirine (RPV) and doravirine (DOR), the second-generation NNRTIs, are three recently approved NNRTIs by the U.S. FDA (United States Food and Drug Administration) that can be effective against HIV variants resistant to first-generation NNRTIs [12,13,14,15]. Integrase strand transfer inhibitors (INSTIs), i.e., raltegravir (RAL), elvitegravir (EVG), dolutegravir (DTG), bictegravir (BIC) and cabotegravir (CAB), are highly potent, with limited toxicity, and have become the cornerstone of modern ART worldwide [16]. Therefore, to control HIV viral replication, two of these new drugs (INSTIs and 2nd-Gen-NNRTI) are sufficient.
In many studies, these drugs, combined in DT, have shown promising results for ART-experienced patients. For example, DT combining raltegravir with etravirine (ANRS 163 ETRAL trial) [17,18], DTG with RPV (SWORD-1 and SWORD-2 studies) [19,20] and long-acting CAB plus RPV (FLAIR and ATLAS clinical trials) [21,22] maintained a high level of viral suppression over 96 weeks in long-term, experienced HIV-infected individuals. Among INSTIs with 2nd-Gen-NNRTI combinations studied, only the long-acting injectable (LAI) RPV + CAB and RPV + DTG combinations have been validated and approved by the U.S. FDA [12].
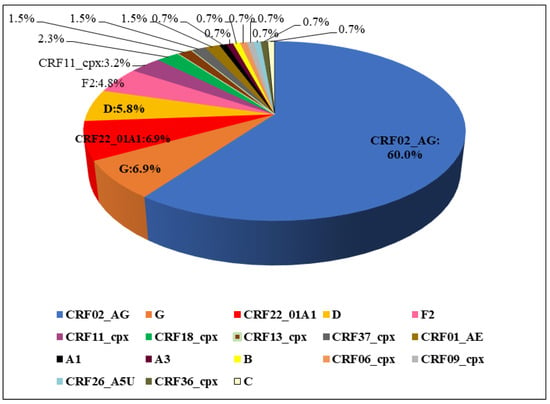
In general, DT is a recommended option for individualized treatment of HIV-1 infection in the Western world, with HIV viral load <50 copies/mL on oral ART, no history of virological failure and no history of NNRTIs drug resistance mutations (RAM). In particular, long-acting therapies are now considered of paramount importance for a number of reasons, such as increasing efficacy, reducing the negative effects of lack of adherence and limiting stigma. For all these reasons, long-acting therapies are seen as a relevant option in low- and middle-income countries, especially in Africa. However, in countries, like Cameroon, there is a large proportion of people with previous exposure to/experiencing failure with NNRTI-containing regimens (and archived NNRTI resistance) [23,24,25] and high viral subtype diversity [26,27]. HIV-infected populations generally have limited access to virological monitoring and/or genotypic resistance testing, which is likely to lead to an accumulation of NNRTI resistance [23,24,25]. For all these reasons, the potential relevance of this new approach needs to be considered in practice in light of the overall rate of failures and resistance to INSTI and/or NNRTI, in order to evaluate which patients—how many are they—have real chances to benefit from this approach.
Therefore, the aim of this study was to explore the potential targets eligible for DT among patients experiencing virological failure, in order to optimize the use of DT in our context. Using HIV genotypic resistance testing, we assessed the predictive efficacy of dual ART combinations (approved, in development, not reported to be in development) based on second-generation INSTI and 2nd-Gen-NNRTI among PLHIV failing their ART in Cameroon. Specifically, we analysed genetic variations in HIV-1 pol sequences to describe the predicted efficacy of DT combining 2nd-INSTIs + 2nd-Gen-NNRTI following treatment failure in Cameroon.
Source link
Davy-Hyacinthe Gouissi Anguechia www.mdpi.com