1. Introduction
Based on the aging population and overall increasing life expectancy, clinicians will be faced with more age-related disorders of the spine. Over the years, spinal fusion surgeries have increased at a higher frequency than other notable in-patient procedures, and the average patient age has also increased for these procedures [
1]. With these developments, concerns are being raised that elderly patients with comorbidities could be at increased risk for complications and worse outcomes after spinal fusion procedures.
Considering this, the concept of frailty has become increasingly recognized as an important issue which can influence clinical outcomes [
2]. Frailty differentiates between chronological and physiological aging, as it describes a decrease in functional reserve capacities, which may be caused by the interaction of progressive age-related decline in physiological systems on the one hand and an increase in chronic diseases on the other [
3]. It is generally defined as a state of vulnerability to stressors, which may be endogenous or exogenous, thereby increasing the risk of negative health-related outcomes [
4]. Due to different definitions of frailty status, the prevalence of who can be considered a “frail patient” varies widely between studies. And yet, a correlation with increasing age has been described. While a higher prevalence of degenerative spine diseases is found within the elderly patient population, complex spine surgeries may offer relief, but they may also carry a higher risk in frail patients, thereby negatively influencing perioperative morbidity [
5].
The literature on the relevance of frailty in patients undergoing transforaminal lumbar interbody fusion (TLIF) surgery is currently limited. TLIF is a frequently performed surgical procedure that utilizes a posterolateral transforaminal approach to the disk, allowing for either an open or a minimally invasive (MIS) decompression and 360° fusion of a spinal motion segment. Higher levels of frailty have been shown to be predictive of readmission, reoperations, any complications, and adjacent segment disease in older patients undergoing single-level TLIF [
6]. Open TLIF in frail patients is also associated with an increased revision rate and the probability to be discharged to a location other than home [
7]. Cage subsidence has been shown to be a potential complication of decompression and fusion surgeries, with age and low bone mineral density (BMD) being significantly associated with worse results, factors which pertain to the frail patient population [
8]. Moreover, cage subsidence may lead to a loss of lumbar lordosis, potentially affecting sagittal alignment parameters negatively. However, to the best of our knowledge, the impact of frailty on cage subsidence—and its subsequent effects on clinical and radiological outcomes following TLIF surgery—has not yet been investigated. With the growing number of frail patients requiring TLIF surgery, this topic remains increasingly relevant.
3. Results
A total of n = 408 patients were identified, who underwent TLIF surgery on 506 levels. 56.1% (n = 229) were female. The non-frail group consisted of n = 276 (67.6%) and the frail group of n = 132 patients (32.4%). The mean age of patients in the frail group was significantly higher (69.2 years vs. 63.6 years,
p < 0.001). There were no significant differences in the gender distribution. Not surprisingly, frail patients were more likely to have higher ASA grades (
p < 0.001) and higher CCI scores (
p < 0.001). Complete baseline demographic information is depicted in
Table 1.
Regarding surgery-specific variables, the overall extent of fusion (mono-/bisegmental vs. multi-level fusion;
p = 0.002) and number of segments fused during the index surgery (2.4 [SD 2.3] vs. 3.0 [SD 2.5],
p = 0.009) was higher in frail patients. Cement augmentation of pedicle screws was more commonly performed in frail patients (33.3% vs. 16.3%,
p < 0.001). No significant differences were observed in the other surgery-specific variables, including the segment at which a TLIF was performed, the length of the procedure, estimated blood loss, and intraoperative AEs (
Table 2).
Frail patients had a longer length of stay (LOS; 12.3 vs. 10.2 days,
p = 0.016), and a higher rate of AEs was detected in frail patients until discharge (40.1% vs. 26.4%,
p = 0.005), as well as at three (25.0% vs. 10.9%,
p = 0.001) and 12 months of follow-up (20.4% vs. 6.5%,
p < 0.001;
Table 3). While no significant difference in the type of AEs (i.e., medical or surgical) was observed at all time points, AEs in frail patients were found to be more often severe (as classified by the TDN score) at three (
p = 0.004) and 12 months follow-up (
p = 0.001). There were no significant differences regarding the degree of intersomatic and posterolateral fusion and presence of clinically relevant pseudarthrosis at any time between both groups (
Table 3). However, CS was diagnosed significantly more often in the frail group at time of discharge (21.5% vs. 15.2%,
p = 0.037) while there was a trend toward higher rates of CS at three (33.1% vs. 24.5%,
p = 0.09) and 12 months postoperatively (33.1% vs. 23.9%,
p = 0.075). Clinical outcomes were inferior in the frail patients both at the three- (
p < 0.001) and the 12-month follow-up (
p = 0.044).
In the univariate logistic regression (
Table 4), frail patients were more likely to experience a postoperative AE until discharge (OR 1.89, 95% CI 1.22–2.92) and at three (OR 1.57, 95% CI 1.07–2.3) and 12 months of follow-up (OR 3.77, 95% CI 1.96–7.24) while the odds of experiencing a favorable outcome at any time postoperatively remained unaffected. The multivariable logistic regression, adjusted for confounders and baseline differences including age, CCI, ASA grades, and numbers of segments fused, showed that frailty was an independent risk factor for postoperative AEs at 12 months (OR 3.44, 95% CI 1.69–6.99), while keeping a tendency for inferior clinical outcomes (OR 0.70, 95% CI 0.44–1.1,
Table 4). The sensitivity analyses showed no significant differences in the overall results and robustness of the linear regression models.
In terms of spinopelvic parameters (
Table 5), frail patients started with more dysbalanced spines preoperatively, represented by lower total lumbar lordosis (LL; 45.9° vs. 50.6°,
p = 0.006), a higher C7 sagittal vertical axis (C7 SVA; 7.0 vs. 4.8 cm,
p = 0.004), and a tendency for a more pronounced mismatch between ideal and actual mismatch (11.5° vs. 8.5°,
p = 0.055). Before discharge, total LL in frail patients was corrected to the extent that no statistically significant differences were observed between the frail and the non-frail patients (LL; 50.6° vs. 50.4°,
p = 0.898). In the postoperative course, total LL significantly decreased in the frail patients at three months (LL; 50.8° vs. 54.4°,
p = 0.011) and 12 months postoperatively (LL; 51.2° vs. 54.5°,
p = 0.032). This resulted in a higher PI–LL mismatch (8.6° vs. 3.6°,
p = 0.006) and in a higher mismatch between ideal and actual LL (8.9° vs. 3.6°,
p = 0.004).
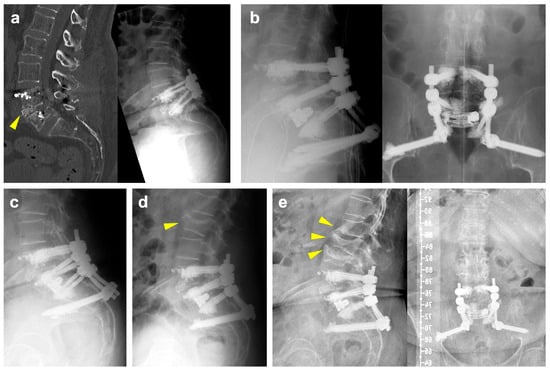
Illustrative Case
The patient is a 71-year-old female with a previous history of degenerative spondylolisthesis at L4/5 with central spinal canal stenosis and associated symptoms of spinal claudication. She therefore underwent TLIF surgery at L4/5 and bilateral decompression at L5/S1 one year prior to the current admission. At the one-year follow-up, she presented with an exacerbation of lumbar pain radiating to the right lower extremity, which was attributed to an adjacent segment degeneration at L5/S1 and a burst fracture of the L5 vertebra (
Figure 1a). Clinically manifest osteoporosis with insufficiency fractures were previously known. Medical treatment with vitamin D and denosumab was previously initiated. Due to unbearable pain, revision surgery was proposed, and extension of the construct distally into the pelvis with TLIF at L5/S1 was planned. Unfortunately, the procedure had to be postponed multiple times due to episodes of cardiac decompensation. As assessed by our anesthesiologists, the preoperative CCI grade was 1 and the ASA grade was 3. Ultimately and following preoperative cardiac optimization, the intervention was performed without intraoperative complications (
Figure 1b). Postoperative imaging revealed cranial cage subsidence (
Figure 1c). Despite this, the patient reported a significant reduction in pain compared to preoperatively. During hospitalization, she developed anemia, which was managed with transfusion of red blood cells. Moreover, she tested positive for influenza. On postop day nine, the patient was discharged to rehabilitation.
A few days after discharge, she was readmitted to cardiology due to subacute myocardial infarction and pulmonary edema. Following an episode of coughing accompanied by sudden onset of back pain, imaging revealed a new fracture of the superior endplate of L2, which did not require surgical intervention (
Figure 1d). At her six-month follow-up, she reported persistent right-sided lumbar pain radiating to the buttock, although improved compared to her preoperative status. Imaging at that time showed new osteoporotic fractures at L1 and L3 (
Figure 1e). Subsequently, the patient refused further follow-up at our clinic due to the long distance from her residence. She currently remains in follow-up with her general practitioner.
4. Discussion
Taking into consideration the increasing age of the global population, clinicians will be faced with more spinal disorders specific to the elderly and the aging of the spine [
15]. To the best of our knowledge, there is a paucity of literature on the influence of frailty on clinical and radiological outcomes in patients undergoing TLIF. Moreover, this is the largest study where expandable interbody spacers were applied—a novel but increasingly used technology. In this study, we were able to demonstrate that frailty has a significant and clinically meaningful negative impact on the likelihood of developing postoperative AEs, while clinical patient outcomes remain influenced to a lesser extent, losing the statistical significance after adjusting for multiple confounding variables. Frailty is certainly an important issue for spine surgeons to be aware of, and the problem we face today is likely to become even more important in the future. Similar to our results in TLIF patients, prior studies have shown that frail and pre-frail patients undergoing posterior lumbar interbody fusion are at higher risk of major complications, readmissions, prolonged hospital stays, and postoperative infections [
16,
17]. Additionally, in anterior lumbar interbody fusion procedures, frailty has been identified as an independent predictor of pulmonary complications, urinary tract infections, pneumonia, and unplanned intubations [
18,
19]. These findings highlight the consistent impact of frailty across different spinal fusion techniques, reinforcing the need for careful preoperative risk assessment and optimization. Topics like meticulous patient selection, including, for example, baseline expectations and psychological capacity to handle unsatisfactory results, as well as patient counseling, including setting appropriate expectations, reviewing the potential risks of surgery, postoperative instructions to limit complications, and long-term follow-up, become increasingly relevant [
20]. Moreover, our current results highlight the need to address factors that may be influenced actively before admitting a patient for surgery, e.g., preoperative medical optimization or prehabilitation [
21].
Our study characterized frail patients to be significantly older than non-frail patients. More importantly, both CCI and ASA grades were significantly higher in the frail patients, which is likely to further contribute to patients’ perioperative vulnerability. Recognition of a patient’s individual vulnerability and initiation of appropriate measures is therefore of utmost importance:
(1) Prehabilitation programs, consisting of preoperative measures, such as general education, exercise, pain education, health behavior counseling, and mindfulness, have been shown to be feasible, reduce medical costs and improve postoperative pain, reduce disability, and improve satisfaction with surgical outcomes [
22].
(2) Multidisciplinary perioperative management approaches, such as the Enhanced Recovery After Surgery (ERAS) approach, include different measures, such as patient education, risk assessment screening, usage of long-lasting local anesthetics, avoidance of urinary catheterization, opioid-limited or opioid-free analgesia, early postoperative mobilization, and prompt nutrition, and have been shown to reduce complications, readmissions, and LOS and improve functional recovery as well as patient-reported outcomes in spine surgery [
23].
(3) Several studies have previously highlighted the importance of postoperative rehabilitation for patients undergoing spinal surgery. However, there is a paucity of studies that specifically focus on frail patients. In elderly patients undergoing lumbar fusion surgery due to degenerative intervertebral disk disease, systemic lower limb rehabilitation led to faster recovery, increased patient satisfaction rate and lesser lower limb deep venous thrombosis [
24]. Also, the ERAS protocol showed that elderly frail patients undergoing multi-level lumbar fusion surgery had significant improvements regarding the recovery of physiological functions and reduction of hospital length of stay [
23]. These findings highlight the importance of future research in rehabilitation protocols for frail patients.
(4) Finally, patient selection and counseling are imperative, as it has previously been shown that a preoperative discrepancy between outcome expectation and actuality led to lower patient satisfaction [
25].
Future studies should also explore the impact of baseline mobility, pain levels, and patient-reported quality of life on outcomes following spinal surgery [
12].
In our frail cohort, patients were not only significantly older but also included a higher proportion of females. Increased age and female sex are known risk factors for the development of osteoporosis. In the presence of conditions characterized by low BMD, such as osteoporosis, cement augmentation of pedicle screws may be indicated in spinal fusion procedures to reduce the risk of hardware failure [
26]. As a result, our findings showed that frail patients were significantly more likely to undergo cement augmentation of pedicle screws than non-frail patients.
Our results further highlight higher rates of CS in frail patients. Age has been identified as a risk factor for the occurrence of CS in patients undergoing open and MIS-TLIF surgery [
27,
28,
29,
30]. This may partially be due to age-related comorbidities and changes in bone metabolism, as well as the use of medication affecting BMD, ultimately resulting in osteoporosis [
31]. Low BMD and osteoporosis, along with cage shape, size, and position, axial compression load of the cage–endplate interface, the amount of cartilaginous endplate removal during surgery, or endplate injury have been identified as risk factors for the occurrence of CS [
32,
33]. Interestingly, the occurrence of CS did not significantly affect the degree of intersomatic fusion or the rate of clinical pseudarthrosis between the frail and the non-frail patients undergoing TLIF surgery. In line with our findings, previous studies have shown that cage subsidence does not necessarily need to be associated with a lower fusion rate or worse clinical outcomes [
34,
35]. We hypothesize that our surgical approach with rigorous removal of the inferior facet joints and cartilage removal provides an additional basis for secondary posterior fusion, as evidenced by the non-significant differences in posterolateral fusion rates between the groups. Ultimately, while preoperative assessment of BMD in patients undergoing spinal fusion surgery is crucial, this is particularly true for patients who are classified as frail. In this retrospective study, we did not collect BMD measurement in all patients, but information on the mean HUs of the adjacent vertebrae was collected and showed no significant differences between the frail and the non-frail patients. Irrespective of the BMD status, however, expandable interbody spacers may be associated with a higher risk of CS [
36]. This has been ascribed to the high forces exerted on the endplates during the expansion process, especially if the segmental release is not thoroughly performed before. Expansion of the interbody spacer should be halted as soon as a good press fit is achieved in order to avoid a breach into the endplates. Ultimately, as seen within our cohort, CS may be one potential reason for the loss of LL on follow-up.
Our study revealed a significantly longer LOS in frail patients, which may partly be explained by the larger extent of the surgery. Frail patients had significantly larger constructs, which consequently harbor a higher probability of risks, complications, and worse outcomes. In line with our findings, previous studies have shown that frail patients undergoing TLIF had a longer LOS and a lesser probability to be discharged home while being more often discharged to locations other than home, such as rehabilitation centers or nursing homes [
7,
16,
37,
38,
39]. Another explanation for the prolonged LOS seen in frail patients may be the significantly higher occurrence and severity of postoperative AEs. Consistent with our results, previous studies have shown that frailty was significantly associated with the occurrence of postoperative AEs in patients undergoing TLIF [
6,
16,
39,
40]. Our univariable analysis indicates that patients were more likely to experience AEs at any time after surgery. However, this finding may reflect significant baseline differences in comorbidities, as measured by the CCI, as well as the extent of the fusion procedure between the frail and the non-frail patients. After adjustment, frail patients were found to be more likely to experience an AE at 12 months postoperatively. And yet, while frail patients in our study were 3.4 times as likely as the non-frail patients to experience a postoperative AE at 12 months, logistic regression analysis did not demonstrate a significant impact of frailty on the odds of having a favorable 12-month outcome (OR 0.71, 95% CI 0.49–1.04,
p = 0.078). Previous studies were able to detect a negative impact of frailty on the clinical outcomes with statistical significance. A retrospective study analyzing N = 488 patients undergoing one- or two-level TLIF surgery showed that severely frail patients had fewer improvements in back pain, with age and CCI also being predictors for inferior outcomes in terms of back and leg pain [
39]. It is important to acknowledge, however, that the latter study focused on severely frail patients only, whereas our frail patient group consisted of a more heterogenous population spanning moderate and severe degrees of frailty.
A possible explanation for the comparable favorable outcome in the frail and the non-frail patients after three and 12 months may be found in the sagittal balance measurements, as it is widely accepted that spinopelvic alignment is important for and correlates with postoperative outcomes [
41]. A positive sagittal imbalance leads to an increased workload on accessory muscles to stay erect during gait and therefore leads to early fatigue and pain especially in the back, buttocks, and thighs [
42]. The C7 SVA has previously been shown to be related to clinical outcomes after spinal fusion surgeries and to be an indicator of health-related quality of life [
43]. Accordingly, in our study, SVA was significantly different between frail and non-frail patients preoperatively, as there were more patients with ASD in the frail cohort. However, there were no significant differences found after three and 12 months, which may explain the similar postoperative outcomes in the multivariate analysis. In line with our findings, a prospective, multi-center, and multi-continental study previously showed that patients over 60 years of age who underwent multi-level spinal fusion had significant improvements in the Oswestry Disability Index after successful procedures, demonstrating that the elderly population may also benefit from ASD surgery, considering age-adjusted alignment goals [
44].
Given our findings, counseling frail patients undergoing TLIF surgery should emphasize their higher likelihood of postoperative complications, including cage subsidence. However, it is important to note that these complications, which often resolve over time, do not necessarily impact long-term outcomes compared to non-frail patients. Therefore, TLIF surgery remains a viable option that can be offered to frail patients if appropriately indicated, with consideration of preoperative optimization strategies to enhance their functional capacity.
Strengths and Limitations
The strengths of this study include the large cohort of consecutively treated patients by a variety of surgeons, as well as a reasonably low missing data burden. The reason for missing data at the three and 12 months follow-up involves the inclusion of patients whose surgery was not long enough ago at the time of the data collection. Three-month follow-up data were available in n = 387 patients (94.9%) and 12-month follow-up data in n = 313 patients (76.7%). Our study revealed clear results with a strikingly high effect size for a topic that is relevant already today, but will be even more important in the future considering the aging population.
The retrospective nature of this study along with its limitations may be considered a weakness. A fourth of patients received another type of interbody fusion in addition to the TLIF during the same procedure, which makes it difficult to establish a direct effect of the intra- or postoperative AEs or the clinical outcome to the TLIF procedure. On the other hand, being inclusive and considering the typical patient cohort of a public, academic spine center, makes our results more generalizable regarding the influence of frailty in spinal (fusion) procedures. Another limitation is the stratification of patients into two groups (frail and non-frail patients), which was decided based on clinical reasoning and was necessary to employ statistical methods like multivariable logistic regression. Sensitivity analyses with slightly modified stratifications of study groups did not reveal much different results. Analyzing each CFI grade separately would have required a much larger sample to keep sufficiently high statistical power. As the results of this study parallel our clinical observations and make sense, we think that having included even “vulnerable” or “mildly frail” patients in the frail cohort is justified.
Moreover, certain surgery-related factors, such as the surgeon’s experience and the chosen surgical approach, were not evaluated in this study and may have a potential influence on outcomes. The use of a single implant type limits the generalizability of our findings to other types of interbody spacers. However, it provided a controlled study environment where the influence of only one specific interbody spacer was examined, thereby reducing the risk for potential confounding. Finally, even though not significantly different between the groups, frail patients had longer operative times and greater blood loss on average, which may have introduced confounding. However, since the operative time and blood loss have shown collinearity with the numbers of segments fused, our multivariable analysis was adjusted for the numbers of segments fused.