1. Introduction
Cervical intraepithelial neoplasia (CIN) is a precancerous condition characterized by abnormal epithelial cell growth in the epithelium of the uterine cervix. CIN is classified into three grades of severity—CIN I, CIN II, and CIN III—depending on the thickness affected by dysplastic cells in the epithelial layer. Loop electrosurgical excision procedure (LEEP) conization is a widely utilized method for managing CIN, offering both diagnostic and therapeutic benefits by excising abnormal tissue. While effective, LEEP conization may reveal lesions more advanced than initially predicted by cytology, underscoring the limitations of traditional cytological screening.
This study explores the relationship between NLR, PLR, MLR, and p16 positivity in patients undergoing LEEP conization for cervical intraepithelial neoplasia. Specifically, we aim to determine whether hematologic markers correlate with p16 expression levels, thereby reflecting disease advancement. By examining this potential association, we seek to evaluate its utility as a prognostic biomarker and its implications for personalized management strategies in cervical cancer care.
2. Materials and Methods
2.1. Patients
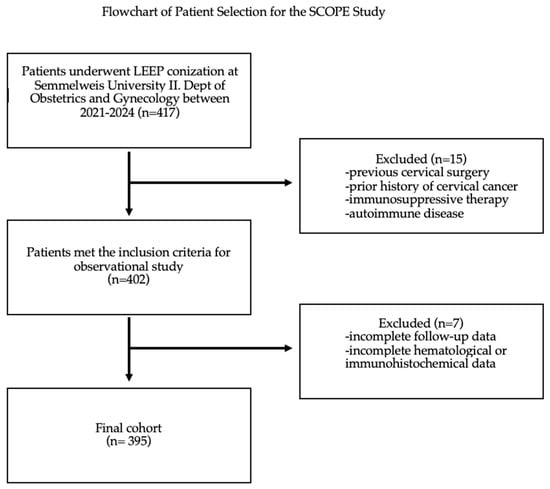
Patients were included in the study if they underwent LEEP conization at the Department of Obstetrics and Gynecology, Semmelweis University; had complete histopathological and hematological data, including NLR, PLR, MLR, and p16 immunohistochemical staining results; and were at least 18 years old at the time of the procedure.
Exclusion criteria were applied to patients who had a prior history of cervical cancer, previous cervical surgery that could have influenced histopathological or hematological findings, or were undergoing or had previously received immunosuppressive therapy. Patients diagnosed with autoimmune diseases that could affect inflammatory markers were also excluded, as were those with incomplete follow-up data or missing relevant clinical information. Additionally, any cases with incomplete hematological or immunohistochemical data necessary for statistical analysis were excluded.
2.2. Characteristics
The sociodemographic characteristics included the patients’ age, calculated by subtracting the year of birth from the year of the surgery. Additional factors included body weight, height, BMI, smoking status, alcohol consumption, known diabetes or hypertension, and the presence of immunological disorders affecting immune function.
All laboratory analyses were conducted in laboratories accredited by the National Accreditation Authority of Hungary, ensuring compliance with quality and accreditation standards. The laboratory parameters included inflammation-related biomarkers, such as neutrophil count, lymphocyte count, monocyte count, and platelet count. From these, specific ratios—neutrophil/lymphocyte ratio (NLR), monocyte/lymphocyte ratio (MLR), and platelet/lymphocyte ratio (PLR)—were calculated. All laboratory tests were performed within one month before surgery.
The screening of cervical dysplasia included the results of cervical cancer screening and HPV status, with a specific focus on the presence of high-risk HPV. Surgical data covered the outcomes of conization and histopathological findings from the conization procedure. These findings encompassed p16 positivity and the presence of glandular involvement. p16 immunohistochemical staining was performed on formalin-fixed, paraffin-embedded histological sections obtained from the LEEP conization specimens.
This study was ethically approved by the Institutional Review Board of Semmelweis University, (SE RKEB: 195/2024).
2.3. Data Management
Data for this retrospective analysis were collected and stored in a dedicated database designed for the SCOPE Study. The database included comprehensive patient records, encompassing sociodemographic, clinical, and laboratory variables. Before analysis, data integrity was ensured through rigorous checks for outliers and inconsistencies, utilizing boxplot visualizations to identify any extreme values that could potentially skew results. Missing data were systematically addressed according to predefined criteria, ensuring that the dataset remained robust for statistical evaluation.
2.4. Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 25.0 (Released 2017. IBM Corp., Armonk, NY, USA). Descriptive statistics, including mean, standard deviation, median, minimum, and maximum values, were calculated for all continuous variables to summarize the characteristics of the study population. The Mann–Whitney U test was employed to compare laboratory values and other variables between groups, particularly assessing differences in neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio (PLR), and lymphocyte/monocyte ratio (LMR) in relation to p16 positivity. A chi-square test was also utilized to evaluate categorical variables. Significance levels were set at p < 0.05.
To further explore the predictive capability of laboratory markers for p16 positivity, receiver operating characteristic (ROC) curves were constructed. This analysis provided insight into the sensitivity and specificity of NLR, PLR, and LMR as potential biomarkers in cervical cancer progression. The results were interpreted to determine optimal cutoff values for clinical application.
4. Discussion
The SCOPE study provides a comprehensive analysis of the relationship between systemic inflammatory markers, specifically the neutrophil/lymphocyte ratio (NLR), and p16 positivity in cervical intraepithelial neoplasia. By elucidating the interplay between systemic inflammation, human papillomavirus (HPV) infection, and the progression of cervical lesions, this research offers significant insights into the underlying pathophysiology and potential prognostic biomarkers in HPV-related cervical disease.
Peripheral blood NLR measurements offer convenience and reproducibility, making them an auxiliary indicator for tumor prognosis.
To ensure that these associations are independent of other conditions potentially elevating systemic inflammatory markers, we also examined the relationship between NLR, PLR, and LMR and factors such as smoking, alcohol consumption, diabetes, and immunological disorders. Our analysis revealed no significant correlations, indicating that the observed associations between systemic inflammation and CIN progression are likely independent of these confounding factors. This strengthens the robustness of our findings by demonstrating that the elevated inflammatory markers are primarily driven by HPV-related disease processes rather than other underlying inflammatory conditions.
The SCOPE study also highlights the challenges associated with defining universal cut-off values for NLR. For instance, while this study observed that all patients with NLR values above 1.31 were HPV-positive, no definitive threshold for normal NLR values could be established, reflecting variations reported in the literature. Future research should focus on standardizing these thresholds to enhance clinical applicability.
Our findings reinforce the link between systemic inflammation and active HPV infections, suggesting that higher NLR values reflect an inflammatory state conducive to viral persistence and progression to CIN or cervical cancer, and demonstrate a clear correlation between NLR and p16 positivity, a surrogate marker for transcriptionally active high-risk HPV. This connection emphasizes the role of systemic inflammation in driving HPV persistence and progression to malignant transformation.
4.1. Strengths and Limitations
This study offers a comprehensive evaluation of systemic inflammatory markers, particularly the neutrophil/lymphocyte ratio, in the context of HPV-related cervical intraepithelial neoplasia. By incorporating a large sample size of 395 patients, robust statistical analyses, and the integration of both hematological and immunohistochemical markers, the findings provide valuable insights into the prognostic potential of NLR. Furthermore, the use of receiver operating characteristic analysis strengthens the diagnostic utility of NLR by quantifying its sensitivity and specificity in predicting p16 positivity. The inclusion of real-world clinical data enhances the study’s applicability to everyday practice, emphasizing the utility of routine laboratory tests in cervical cancer management. As a retrospective study, the analysis is subject to inherent limitations, including potential selection and information biases. Unlike randomized controlled trials, this study lacks randomization and prospective data collection, which may impact the generalizability of the findings. Additionally, while the study identifies significant associations, causality cannot be established due to the study design.
4.2. Implication for Practice
NLR, as a cost-effective and widely accessible marker, provides an additional layer of diagnostic precision when combined with p16 immunostaining. This can enhance the early detection of high-grade lesions. Importantly, routine blood tests, including NLR, are universally available, require no additional cost, and are already part of standard preoperative assessments. In resource-limited settings, where advanced adjunctive tests such as p16/Ki-67 dual staining might not be affordable and diagnostic pathways may still heavily rely on the sensitivity of the Pap test alone, NLR emerges as a valuable, simple, repeatable, and promising tool. Its integration into cervical cancer screening and management protocols could aid in early disease detection, risk stratification, and treatment monitoring with minimal financial burden on healthcare systems. This highlights the clinical relevance of our findings, particularly in settings where cost-effective and accessible diagnostic solutions are most needed.
4.3. Future Perspective
Future perspectives include the need for longitudinal studies to evaluate the predictive accuracy of NLR over time and its role in guiding therapeutic decisions. Investigating interventions targeting systemic inflammation could also provide valuable insights into altering the disease trajectory of HPV-related cervical pathology.
Source link
Zsófia Tóth www.mdpi.com