1. Introduction
Innovation is key to the advancement of medicine and subsequent improvement in patient care [
1]. This is particularly true in surgery, where pioneering techniques have transformed operative management from historically highly risky, peri-morbid, and disfiguring procedures to contemporary low-risk and minimally invasive approaches [
2]. There is a delicate balance between enabling innovation and minimizing patient harm [
3]. However, the pathway to surgical innovation is often fraught with numerous barriers, including the need to demonstrate not only clinical effectiveness but also cost-effectiveness and safety. Regulatory requirements from agencies such as the Food and Drug Administration (FDA), European Medicines Agency (EMA), and National Institute for Health and Care Excellence (NICE) further complicate this landscape, each imposing distinct standards and hurdles that must be navigated before new techniques can be widely adopted [
4].
A critical factor contributing to the propensity of journals to accept publications on novel surgical techniques is the number of cases included in the study. Higher case numbers often provide stronger evidence for the efficacy and safety of a procedure, making it more likely to gain acceptance from both peer-reviewed journals and regulatory bodies [
5,
6]. This emphasis on case numbers reflects a broader shift towards evidence-based practice, where substantial case series are needed to justify the adoption of new procedures, especially those that may involve higher costs or increased surgical risks.
4. Results and Discussion
A total of 68 publications describing pioneering techniques in urology were identified (
Appendix A). These included 16 isolated case reports and 52 case series. Among the case series, 22 involved small cohorts with 2 to 10 cases, while 30 featured larger cohorts with more than 10 cases. Initial analysis was performed by grouping publications in chronological ordinal groups, and ordinal logistical regression was performed. Pioneering urological techniques were then split into six discrete domains including uro-oncology (bladder), uro-oncology (prostate), uro-oncology (kidney), reconstructive urology (upper tract), reconstructive urology (lower tract), and endourology.
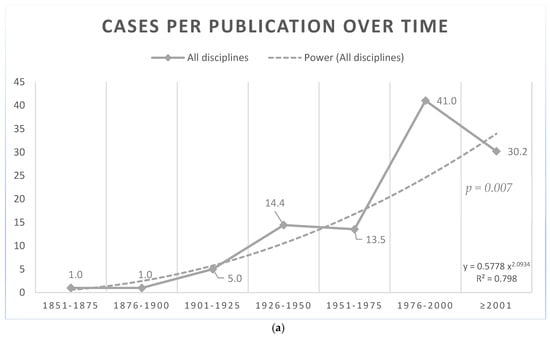
Prior to 1901, techniques in urology were published as solitary case reports (mean cases per publication [CPP] = 1) (
Figure 1a). Publications from 1901 onwards demonstrated a gradual increase in cases per publication (R
2 = 0.798, OR = 6.29 [95% CI: 2.57 to 10.02],
p = 0.007) (
Figure 1a). This can be largely attributed to the transformative nature of historical procedures allowing for the surgical technique itself to be a focus of the publication. Procedures such as open radical nephrectomy and open radical prostatectomy were considered transformative as they changed surgical management drastically. These procedures were widely adopted at the time, as their benefits were evident. In contrast, modifications to existing, widely adopted procedures often showed only incremental benefits. As such larger case series are often required to demonstrate the additional benefits derived from novel procedures and justify increased costs or surgical risks. A clear example was seen comparing the introduction of transvesical prostatectomy (1887, 1 case) to the Transurethral Resection of the Prostate (TURP) (1926, 46 cases) and to the Holmium Laser Enucleation of the Prostate (HoLEP) (1995, 110 cases) (
Appendix A).
When split into distinct domains, the findings were more heterogenous (
Figure 1b). Whilst the general trend was an increase in CPP with time, recent surgical innovations paired with technological innovations have not followed this. This is well demonstrated by endourological publications where CPP peaked at 110 for the period 1976–2000 and subsequently decreased to 12 CPP from 2001 onwards. This was due to the low number of cases published in the initial case series of recent endourological procedures paired with technological innovation for the treatment of benign prostatic hypertrophy (BPH) such as Urolift and the Greenlight Photovaporization of Prostate and Rezum (
Appendix A). A similar pattern was seen in reconstructive urological procedures, with the highest CPP seen in the period 1951–2000.
Our results reveal that many transformative surgical techniques were initially reported as isolated case studies or small series, underscoring the primacy of innovation over publication volume. This observation highlights the need for flexible publication standards that emphasize methodological rigor and robust peer review rather than adherence to arbitrary thresholds such as minimum case numbers. While larger case series offer strong evidence for the safety and efficacy of novel techniques, they are not without limitations. The extended time required to accrue substantial cohorts, particularly in centers with lower procedural volumes, can delay the dissemination and clinical adoption of potentially groundbreaking innovations. Additionally, the financial and logistical burdens associated with conducting large-scale studies may disproportionately affect resource-limited settings, thereby restricting the diversity and inclusivity of contributions to the surgical literature.
The Idea, Development, Exploration, Assessment, Long-term (IDEAL) framework, introduced in 2009, provides a structured approach to the optimal generation of evidence for surgical innovation. It outlines five stages: Idea, Development, Exploration, Assessment, and Long-term, guiding the progression of a novel procedure from its initial description through evaluation and exploration to its long-term study [
8]. The IDEAL framework adds significant value by improving the quality of evidence for new surgical interventions. It specifies the appropriate study designs and reporting requirements at each stage, ensuring robust evaluation and collective learning. Additionally, it helps to determine when to advance to higher levels of evidence, such as randomized clinical trials. By encouraging standardization and transparency, the framework promotes safe, efficient, and evidence-based surgical innovation [
4,
8]. The integration of frameworks such as IDEAL can significantly enhance the systematic evaluation of novel techniques. However, maintaining flexibility within the publication process remains crucial. Journals should evaluate each submission on its individual merits, employing rigorous peer review to address potential limitations inherent in smaller studies. This approach fosters an environment where innovation can progress without compromising patient safety or the scientific rigor essential to maintaining the integrity of the evidence base.
This study’s limitations include reliance on major databases and by selecting English-language-only publications. To mitigate this selection bias, the authors performed independent literature searches with multiple reviewers to reduce oversight and ensure consistency through centralized adjudication. A broad search strategy, using various databases (PubMed, Ovid, and Scopus) and diverse keywords, was employed to capture a wider range of pioneering techniques. Additionally, reference chasing and the inclusion of non-English publications aimed to minimize language bias. The inclusion criteria, developed with a senior urologist and cross-referenced with standard texts, ensured a comprehensive and rigorous search process, further addressing potential biases in study selection.