1. Introduction
Nearly five years after the first cases of people with COVID-19, this health problem continues to be of interest for clinical care and research. The 2020 pandemic and its subsequent consequences, in all spheres of life, have highlighted the fragility of health systems and the importance of establishing sociopolitical and health strategies to protect the most vulnerable. In this sense, the concept of vulnerability and the tools that make it possible to measure this vulnerability in individuals and population groups is key to inform clinical prioritization decisions.
In a society marked by knowledge management, these tools must collect and analyse the data available in health system dashboards to return meaningful information that distinguishes individuals, families and/or communities according to their level of vulnerability.
In this sense, the general objective of this research is to determine the level of community vulnerability of a population group by means of health indicators from the electronic health record of Primary Care.
1.1. Impact of the COVID-19 Pandemic on Population and Healthcare
1.2. Care Vulnerability Index (CVI)
The CVI is defined by the BVCs that define the person and their vulnerability, in relation to the characteristics of the environment that represent the risk. The union of both, vulnerability and risk, gives rise to the predisposition to suffer care problems.
The CVI has been used to calculate individual or family group vulnerability, but it was never adapted to analyse community vulnerability.
1.3. Primary Care Health Indicators
2. Materials and Methods
2.1. Scope
2.2. Period
The data collected correspond to the period March 2023–January 2024.
2.3. Study Sample
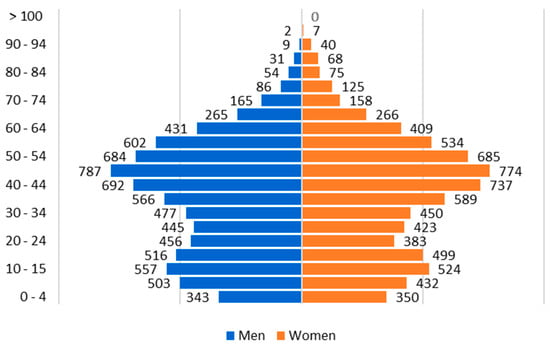
The sample of the study population are the persons assigned to a Family and Community Nurse Specialist at Healthcare Centre Meco. This professional has a total of 2106 people assigned to him as of 25 February 2024, corresponding to the municipality of Meco, but also to the other municipalities mentioned above.
The study sample includes people from all over the municipality without limitations of any condition because the Primary Care nursing service is a reference for people of any age or condition.
The sample size calculation on the total population of Meco (14,856 people) is 638 people for a confidence interval (IC) of 99% and a margin of error of 5%. Thus, the study sample includes 2106 people, which ensures representativeness. In addition, the age and sex distribution are similar to the population pyramid of Meco. The study sample under 15 years of age is 13.58%, between 15 and 64 years of age is 76.73% and from 65 years of age is 9.69%. The distribution by sex is similar, with 49.91% men and 50.09% women.
2.4. Process
This study carries out a methodological process that applies theory and practice. From the abstraction level, this study uses a Care ontology (Knowledge Model about Person Care) as a framework through a model (Vulnerability Model). This model is put into clinical practice through an assessment instrument (CVI).
On the other hand, from the clinical level in a real situation, this study uses a population sample from a town in Madrid where the first level of care uses a single electronic clinical history per person with a structure common to the entire region. This information system is linked to a dashboard with indicators common to all health centres that allow monitoring relevant information on more than 3 million Madrid residents.
2.4.1. Selection of e-SOAP Indicators
The first step is to select the indicators through which the data reflecting the vulnerability situation of the study sample are obtained, its means, to identify indicators related to the BVC.
Phase I Screening. The objective of this first phase is a screening to identify the indicators of the sample universe for the study. This phase is divided into two rounds. Round 1: Exclude indicators not directly linked to the clinical activity of the reference nurse. These support units are Palliative Home Care Support Team (PHCST), Midwife, Physiotherapy and Oral and Dental health. Round 2: Exclude indicators not operational at the time of study. Indicators that are in e-SOAP but do not have measurement data for the study period.
Phase II Eligibility. This phase aims to identify the objectives specific to the purpose of the study, so three rounds of exclusion are applied. Round 3: Exclude indicators on the efficiency of the professional’s activity that do not report on the health outcomes of the person but report on health activity processes. For example, implementation of care plans, follow-up control of patients with a specific chronic disease. Round 4: Exclude indicators linked to processes regulated by regulations that have an obligation of equal care for all persons and, therefore, do not allow discriminating the person’s level of care. For example, follow-up of polymedicated program, vaccination schedule. Round 5: Exclude indicators associated with the COVID-19 process that arise specifically ad hoc during the pandemic because they have shown changes in the definition of the indicator, as well as in the ability to identify the actual population data assigned to the referring nurse professional, because individuals were cared for in centralized resources or at their place of work.
Phase III Inclusion. The last phase aims to determine the study sample through the definitions of the indicators in order to minimize the computational cost of calculating the CVI and thus optimize the efficiency of the study. This phase has only one round where four exclusion criteria are applied: indicators composed of two lamps; for example, percentage of people with arterial hypertension with ventricular hypertrophy, or percentage of people with ischemic heart disease and/or stroke with controlled blood pressure levels; indicators associated with administrative processes; for example, indicators on care plans for specific populations, frequentation of the health system; indicators associated with pharmacological treatment; for example, patients with heart disease treated with statins and indicators associated with healthcare processes. For example, good control, effective management, overuse of test strips for measuring blood glucose, pressure ulcers in bedridden persons.
2.4.2. Relationship of the Indicators to the Basic Variables of Care
The sample of selected indicators is associated to each of the BVCs by means of a content analysis. This content analysis includes the definition of each BVC and the definition of the indicator to establish whether or not an indicator provides information on that BVC.
The first step is to create a Karnaugh table that shows the relationship between each indicator and BVC. Once the relationship is established, the study details the range value of the BVC to which the indicator is linked.
For example, the indicator “patients with arterial hypertension with age-adjusted blood pressure control” is related to the BVC “Physical limitation”, and, specifically, this indicator reports the range value “Compensated” physical limitation. However, the indicator “persons who engage in risky alcohol consumption” is related to the BVC “Physical limitation” and range value “Not compensated”.
At the end of this detailed relationship at the BVC rank value level, each indicator is linked to a vulnerability score according to the CVI. Continuing with the previous examples, the indicator “patients with arterial hypertension with age-adjusted blood pressure control” has a score of 0.5 and the indicator “Persons with risky alcohol consumption” has a score of 1; both out of a maximum of 1. This score reflects that persons with risky alcohol consumption are more vulnerable than persons with controlled hypertension, but both are higher than healthy people without chronic disease or toxic habits.
For this research, the BVC Age score (used as Life stage) requires adaptation because the indicators do not share the same life stage divisions according to years. In this sense, the study uses two rank values: Life Stage Childhood–Adolescence and Life Stage Youth–Elderly. The score for each stage is the arithmetic mean of the scores for the life stages it encompasses. The Childhood–Adolescence life stage scores 0.75 points and the Youth–Elderly life stage scores 0.25 points out of a maximum of 1 point as the highest level of vulnerability.
This step allows us to start working from the DCM, specifically, the Algebraic Mode.
2.4.3. Weighting by Vulnerability Correction Factor
The selected indicators refer to a part of the total population sample studied, i.e., the indicators report on healthcare outcomes of a group of people in the sample, but do not report on the total number of people assigned to the nurse (n = 2106 people).
In addition, these specific groups are different for each indicator, so the scores from the previous phase must be adjusted. Furthermore, each indicator is measured on more than one occasion in the period under study, so it is necessary to estimate a population mean for each indicator.
The number of people included in each indicator (the proportion of the total population) is the average of the number of people included in the indicator at each cut-off during the nine-month study period. For example, if an indicator has three measurements in the study period (March 2023–January 2024), the study adds the number of people included in each measurement and divides by three.
This correction factor is called the Vulnerability Correction Factor (VCF) and allows estimating a weight adjusted to the actual population analysed.
The population-adjusted weight (adjusted score) is obtained by multiplying the score given in the previous phase by the proportion of the population included in the indicator in relation to the total study sample.
Population-adjusted weight = (CVI points of the indicator × VCF)/total number of people in the study sample.
2.4.4. Calculation of Vulnerability Index
The last phase of the study calculates the CVI.
First, the average score of each BVC is calculated using the arithmetic mean of the scores (once the VCF has been applied) of all the indicators that are associated with the BVC.
Cluster 1 = ((Life Stage + Developmental Status)/2) × 5
Cluster 2 = ((Perception of gender limitation + Sociocultural integration)/2) × 1
Cluster 3 = ((Family care system + Individual care system)/2) × 3
Cluster 4 = ((Physical limitations + Cognitive limitations + Sensory limitations)/3) × 4
Cluster 5 = ((Environmental Factors + Material Resources + Time Resource)/3) × 2
The final CVI score is the sum of the scores of all clusters, with the final range of scores being between 0 points (Lowest vulnerability) and 15 points (Highest vulnerability)
2.5. Data Analysis
The research applies the Excel® program for the electronic notebook for data collection, score analysis and calculation of the CVI.
The process meets validity and reliability criteria. The methods used include the collection of data from the entire sample, from an official data source, with anonymous data and applying correction factors to the score according to the number of persons in the sample included in each indicator. In this sense, the data are obtained from a single source of data, official and unique for the entire Community of Madrid, with direct access to the data and the need for processing for the study.
2.6. Ethical Considerations
The research did not collect or identify individual persons (researchers did not make queries from the Autonomous Community Personal Identification Code) at any time during the consultation carried out in the clinical information system referring to the electronic clinical record. Researchers could not identify personal data because they had group-level general data as a group of persons attended by a health professional.
The Research Ethics Committee of the Príncipe de Asturias University Hospital assessed and approved the research study on 31 January 2024 (Code: OE 06/2024).
3. Results
The results of this study are shown below in order:
3.1. Indicators Selection
After the analysis and screening process, the sample has a total of 18 indicators.
People with severe or total functional impairment (Barthel ≤60) with care plans.
Management of hypercholesterolemia in secondary prevention of ischemic heart disease
Chronic patients in health institutions with assigned NI (≥70 years)
Patients with ischemic heart disease and controlled blood pressure levels
Diabetic patients with adequate age-adjusted glycated haemoglobin control.
Patients with diabetes and controlled blood pressure levels
Patients with chronic kidney disease and controlled blood pressure levels adjusted for age and albuminuria.
Patients with stroke and controlled blood pressure levels.
Patients with heart failure and controlled blood pressure levels.
Patients with arterial hypertension with age-adjusted blood pressure control
People with healthy eating
Persons with risky alcohol consumption.
Smokers
People who practice physical exercise
Obese children
Overweight children
Children with healthy eating
Children who practice physical exercise
3.2. Relationship of the Indicators to the Basic Variables of Care
The relationship between each indicator and the BVC uses the indicator label, the formula, the definition and, especially, the inclusion and exclusion criteria that appear in the indicator sheets.
One criterion widely used by indicators is age. Indicators usually make explicit to which type of population they are limited by age. Therefore, the sample is not the entire nursing population, but only the adult, paediatric or elderly population. This condition already establishes a relationship between the indicator and the BVC “Life Stage” and the results reflect which life stage, and which score it corresponds to for the calculation of the CVI. On the other hand, the indicators do not provide information on the BVC “Developmental State” and therefore the results show this BVC without relationships to indicators.
Regarding the BVC “Sociocultural integration”, the people included in these indicators were considered to be enculturated, because they had attended the health system and therefore communication and understanding between the person and the health professional was possible.
Regarding the BVC “Family system of care”, it relates to any person who is dependent for his/her care and needs the help of another person to meet his/her needs. Further, on the BVC “Individual system of care”, all the indicators give information on some sphere of care for these people, whether it is about living habits or about the degree of control of their basic disease.
Another area is healthcare limitations. BVC “Physical limitations”: all indicators that refer to diseases that affect the physical or physiological level of the person, as well as those related to mobility limitations. BVC “Cognitive limitations”: all indicators that refer to diseases or life situations that affect the ability to understand and make decisions. BVC “Sensory limitations”: all indicators referring to diseases or health processes that alter any of the senses (sight, hearing, taste, smell, touch).
As for the BVC “Environmental factors”, it is favourable because the geographical area of study does not have limitations for self-care. The area has electricity, water, healthy streets, green areas, security systems (local police), supermarkets, schools, libraries and parks; they are not municipalities that are undergoing natural disasters or are at war, in which case it would be considered a hindering environment for self-care.
Finally, the BVC “Material resources” and BVC “Time resource” are considered favourable based on the municipality’s data. Meco is within Madrid and has a public health system with a health centre in the area and a nearby hospital, as well as other resources for social care or dependent people or people with different types of needs. The population is generally adult, active and there are no unemployment or similar problems that could be interpreted as a difficulty of resources or time.
Among the results, it is noteworthy that the BVC Sex shows no relationship (NR) with any indicator. This BVC is included in the initial analysis but is not part of the CVI because it does not condition the possibility of suffering harm. Perception of limitation associated with gender is the BVC that is included in the CVI.
3.3. Weighting by Vulnerability Correction Factor (VCF)
The scores obtained in the previous phase are adjusted by means of the VCF that considers the difference in the number of persons represented by each selected indicator.
3.4. Calculation of Care Vulnerability Index (CVI)
Finally, this study calculates the CVI by applying the formula presented in the methodology that groups the BVCs into five clusters, which have a different score from 1 to 5 points and a final result between 0 and 15 points.
4. Discussion
This study achieves its main objective to determine the level of community vulnerability of a population through health indicators.
In this regard, similar publications on community vulnerability coincide in the type of variables under study.
4.1. Limitations of the Study and Future Lines
This research has some limitations that should be pointed out.
The limitation of a period of time can also lead to a bias in the data if it coincides with certain circumstances; for example, collection during the pandemic period would result in low levels of registrations for attention to chronic processes and high levels for acute respiratory processes. The study was conducted over a nine-month period and was expected to cover a large part of the reference population sample.
However, in the Community of Madrid Health Service, all individuals are assigned a nurse and a physician at the Primary Care level. This professional is the reference for selecting the sample in a specific health centre. However, the clinical history is not unique to a professional. The clinical history is unique and the same for each person throughout life and for all the professionals who provide care in Primary Care. In this sense, although the study uses a study sample with reference to a specialist nurse, the indicators studied are the result of all the health interventions of the person throughout life, with any health professional and in any of the health centres in Madrid. The recording biases that appear if only what is written by one professional is studied are minimized because the study collects records from different professionals and at different times of life.
In the future, these limitations offer new lines of research with studies in different population groups, or in the same group, but with annual cutoffs over time. Likewise, future studies should delve into the validation of the selected health indicators and evaluate whether the defined CVI would improve the number of indicators from a cost-effective point of view in order to design and implement a technological application of the community CVI.
4.2. Relevance to Clinical Practice
The CVI has a history of practical usefulness, but it has never been applied from a group or community point of view.
This study reflects the value of the CVI and the opportunity to work with standardized health indicators defined and available in all centres of a healthcare network that serves more than 6.5 million people of different nationalities.
The use of health indicators as a source of data for calculating community vulnerability shows that technological applications can be used effectively and efficiently even in adverse environments, for example, following health crises such as COVID-19.
Replication of the study with different population groups, in the same period of time, allows comparison of the level of vulnerability managed by each nurse or other health professionals. In addition, it provides a continuous programmed assessment of the level of vulnerability of population groups and communities, which can be used to predict the needs of the population in the face of new pandemics and to prioritize efforts in the distribution of health resources.
Likewise, replicating the study constantly over time makes it possible to evaluate and monitor the evolution of the population’s health, the effectiveness of the professional’s actions and the history of care in a community.
This should be the reference point for further integration of these health technologies in the design and delivery of post-pandemic and inter-pandemic healthcare, as it allows the identification of vulnerable populations and the prioritization of healthcare delivery to those most in need.
This is of great interest in the Primary Care and community healthcare setting, since care specialists such as family and community nurses can prioritize their clinical interventions towards care actions focused on health education, assistance or accompaniment of their population, depending on the level of vulnerability of the population to which they provide care.
The results of the CVI make it possible to identify which populations are more vulnerable and require more resources; or which professionals are assigned to the most vulnerable populations. From a management point of view, the calculation of the CVI enables the generation of dashboard systems, to homogenize the burden of care of the different professionals within the same health team or allows the most vulnerable populations to be assigned to the most highly trained specialist professionals.
The results of this study lay the basis for a significant transformation of healthcare following the COVID-19 pandemic, so that healthcare systems and their professionals can be better prepared to meet the future needs of the population after suffering global health crises such as COVID-19.
For all these reasons, the application of the CVI to a population makes it possible to determine its vulnerability situation, in order to specifically prioritize community health promotion, prevention and rehabilitation activities, at the health, economic and/or social levels in post-pandemic periods.
5. Conclusions
COVID-19 is still active today and, therefore, knowing the health situation of populations in post-pandemic times allows us to discover the new population needs, as well as the pending needs to be covered by the health system.
After a pandemic crisis situation such as COVID-19, the availability of updated data on the community health situation is key for health management in post-pandemic situations and subsequent strategic planning actions at different levels.
Vulnerability is an individual but also a collective concept where a group expresses a level of vulnerability inherent to its own individual and community characteristics.
The CVI, defined in previous studies at the individual or family level, can be calculated for an entire community. The knowledge model is the same in both cases because it uses the same Vulnerability Model and the same data source. A Specific Dashboard proves to be sufficient and adequate for obtaining the indicators provided by the data. Therefore, this community vulnerability can be monitored through the Specific Dashboard (included in e-SOAP) with a set of indicators available to all Primary Care nurses in Madrid (Spain).
The calculation of community vulnerability after the COVID-19 pandemic provides objective data on the prioritization of resources to the most vulnerable populations, at the health, economic and/or social levels.
The application of the CVI in post-pandemic and inter-pandemic situations also makes it possible to predict future population needs in the event of the emergence of new global health crises.
This is possible thanks to the availability of a sequence of health-vulnerability benchmarks with which to compare the health evolution of the population, and to be able to manage, plan and prioritize healthcare resources efficiently; since this study is carried out with standardized indicators, available and common to all professionals in a national health region, it is possible to replicate in those health services that have computerized medical records.
In conclusion, community vulnerability is the set of vulnerabilities of the people who make up a community. This definition assumes the relationship between two concepts: vulnerability and community.
Vulnerability is understood as the inherent quality of people to be injured or susceptible to physical or moral harm and it is particularly sensitive to health crises such as pandemics. This is because vulnerability in the field of health conditions the balance of people’s needs and competencies for their own care and the care of others, including the care of their environment.
But the study of vulnerability, as evidenced by COVID-19, must be carried out not only on an individual level, but also on a group or community level.
By community we mean a group of people, whether or not connected temporally or spatially, who share a common purpose, interest, values and principles, identified through common care habits, which have an impact on their health and life. The COVID-19 pandemic repositioned the value of the community health approach to address global health problems.
Therefore, the measurement and monitoring of community vulnerability, through the Community Vulnerability Index, is an essential tool in community health diagnoses and makes it possible to be prepared for future COVID-19 outbreaks or other global health crisis situations.
Source link
Andrea Sierra-Ortega www.mdpi.com