1. Introduction
Type 2 diabetes is a significant public health problem in the United States, with 38 million people diagnosed and approximately 98 million people at increased risk [
1]. In addition, each year approximately 5–10% of at-risk individuals will develop type 2 diabetes without lifestyle modifications [
2]. Effective prevention resources that support changes in nutrition and physical activity, such as the National Diabetes Prevention Program (National DPP), are essential for reducing risk for type 2 diabetes. However, individual and contextual factors can affect participation in prevention activities regardless of the prevention resource format, and therefore understanding the impact of these factors on participant experiences is important. The overall goal of this study was to understand National DPP implementation in rural workplace settings. Specifically, to examine factors that influenced individuals’ outcomes and participation, including program-specific outcomes (e.g., weight) and retention, and participants’ perceptions of the program itself.
The National DPP promotes lifestyle change for type 2 diabetes risk reduction through education, skills, and support [
3]. A key component of the National DPP is a structured, evidence-based, year-long lifestyle change program to prevent or delay the onset of type 2 diabetes in adults with prediabetes or at high risk of developing type 2 diabetes. The National DPP lifestyle change program is founded on the science of the Diabetes Prevention Program research study [
4] and subsequent translation studies, which showed that making modest behavior changes helped adults with prediabetes lose 5% to 7% of their body weight and reduce their risk of developing type 2 diabetes by 58% (71% for people over 60 years old). The program is group-based, facilitated by a trained Lifestyle Coach, and uses a CDC-approved curriculum. The curriculum supports regular interaction between the Lifestyle Coach and participants, builds peer support, and focuses on behavior modification through healthy eating, increasing physical activity, and managing stress. The program may be delivered in person, online, via distance learning, or through a combination of these delivery modes.
The positive impact and effectiveness of the National DPP have been extensively researched [
3,
5]. In addition, the National DPP has been translated in real-world [
6] and workplace [
7] settings. The program is found to be effective (i.e., participant weight loss) when it is adapted to context and population. However, further research is needed to understand individual and contextual factors unrelated to program delivery, such as recruitment of at-risk individuals and retention of participants, that affect translation and implementation. For example, many individuals are not aware of their risk status or options for prevention [
8]. In addition, once at-risk individuals participate in a National DPP, their continued involvement in the program is often associated with motivation for weight loss [
3] and success with weight loss and physical activity [
9], rather than program delivery or format. Examining participant experiences with and perceptions of the DPP may provide valuable insight into program implementation.
Participant issues with meeting the National DPP outcome goals may be due to individual factors related to behavior change. Some of the long-term challenges identified in participants’ ability to maintain behaviors and skills learned in the DPP include difficulties with independent nutrition, physical activity monitoring, accountability, and diminishing motivation [
10]. However, adherence to lifestyle change activities and interventions is a complex process impacted by contextual and behavioral factors as well as individual readiness or motivation for change [
11]. That is, individuals may receive messages and information about the benefits of behavior change and not make any changes. In addition, due to the complexities of change, individual behavior change can be very difficult to predict. Given that the National DPP focuses primarily on the importance of weight loss, other physical and mental health indicators of success may not be adequately conceptualized as critical for behavior change within the National DPP. To address this, it is essential for National DPP implementation research to consider factors that may influence retention, effectiveness, and sustainability. For example, research should envision updates to the curriculum and complementary approaches within, and enhancements to, the existing programming that take additional characteristics of behavior change into account [
12,
13].
Participant engagement in the National DPP sessions and curriculum can also affect achievement of program outcome goals. However, various factors associated with lifestyle change activities influence how at-risk individuals meaningfully participate in prevention interventions and eventually experience success. Psychosocial factors may be the impetus behind positive health outcomes of lifestyle change and provide meaningful information for understanding individual participation in a lifestyle change program. Self-efficacy is associated with positive changes in diet and waist circumference [
14]; problem-solving skills beneficially impact weight loss maintenance [
10]; goal setting, social support, and use of incentives are related to effective physical activity adherence [
15,
16]; prior success and increased motivation are related to successful weight loss [
17,
18]. Examining the role of these factors in the National DPP may provide valuable insight into dissemination, implementation, and tailoring of the program in different populations and contexts. An important next step toward acknowledging the importance of these factors and expanding the success of the National DPP is to understand the individual experiences of participants in underserved areas.
The positive outcomes associated with participation in the National DPP have been established through research in mostly urban and well-supported organizations. Therefore, research examining translation in rural populations is important. Rural areas have a greater diagnosed diabetes prevalence of 12.8% compared to 10.1% in metro areas [
19] due to a variety of factors, including disparities in access to health-promoting behaviors and health care resources [
20]. A major impediment to type 2 diabetes risk reduction for rural individuals is limited access to prevention resources and support [
21]. A study of National DPP implementation in rural and urban areas of the United States found fewer programs in rural (14.6%) versus urban (48.4%) counties [
22]. Accessibility barriers limit the likelihood of individuals to achieve positive health outcomes associated with prevention efforts. As such, it is imperative to understand how to implement and maintain the National DPP in rural settings. Specifically, investigations into DPP translation in rural areas should determine aspects of the program that may need to adapt by learning about common barriers and group preferences [
23]. Research that examines the complexities of lifestyle change affecting program implementation will lead to at-risk individual success with long-term maintenance of changes learned in the National DPP. Therefore, the purpose of this study was to understand National DPP implementation in two rural workplace settings and the factors that influenced participants’ outcomes and involvement in the program.
2. Methods
2.1. Design
The National DPP was implemented in two rural workplace settings. The first National DPP (Technology-Augmented DPP [Setting 1]; East Carolina University [ECU; Setting 2]) occurred in 2016 with the goal of understanding the role of psychosocial factors in relation to National DPP outcomes. ECU is located in a metro area (Greenville, NC, urban core of 50,000 or more people) and surrounded by 4 rural counties [
19,
24]. In addition, ECU’s workforce is comprised of individuals living in rural areas surrounding the city, and the university serves Eastern North Carolina, which faces significant health disparities, including higher rates of type 2 diabetes, low education levels, and poverty compared to the rest of the country [
25,
26]. The second National DPP (Hybrid-Format DPP [Setting 2]; University of Wyoming [UW]) occurred in 2022 with the goal of understanding factors that impact participant perceptions of and satisfaction with the program. The UW is located in a rural micro area (Laramie, WY, urban core of 10,000–49,999 people) [
19,
24]. The institutional review board at both universities approved all study procedures (ECU protocol # UMCIRB 15-001054; UW protocols #20151103JT00964 and #20220729JT03368).
2.2. Technology-Augmented DPP (Setting 1)
Participants: University employees between the ages of 25 and 64 years, with a body mass index (BMI) ≥ 25.0 kg/m2, sedentary (defined as <150 min/week of physical activity), passed a Physical Activity Readiness questionnaire, and were not diagnosed with type 2 diabetes, participated in the program. Individuals who agreed to participate read and signed the consent form prior to completing study measures. Data were obtained from 47 participants who completed the program.
Procedure: The Technology-Augmented DPP followed the CDC-approved curriculum with the addition of a social media component. The program was facilitated by a trained Lifestyle Coach. Each participant joined a Facebook group, specifically designed for their National DPP sessions (e.g., Tuesdays at lunchtime). The Facebook group was used by participants to share recipes, tips, and articles and post questions or feedback. The Lifestyle Coach encouraged participants to post their diet and physical activity goals for the coming week and provided seeder questions, relating to that week’s lesson, for participant response. On alternate weeks, participants did not meet in person and instead received a health education email. Emails provided motivational tips and techniques based on that week’s lesson but did not provide any participant-specific feedback. Measures were obtained at the beginning and end of the program. Researchers also completed weekly process evaluations by asking participants about their experiences with the sessions.
Measures: The Lifestyle-Health-Related Self-Concept (HRSC) evaluates the relationship between self-concept and health behavior and provides insight into the role of psychosocial factors relevant to type 2 diabetes prevention [
27]. Factors of Lifestyle-HRSC assess individual perceptions of DPP components such as improving diet and physical activity, identifying social support, identifying barriers to healthy lifestyles, and overcoming barriers. Lifestyle-HRSC was measured at baseline and endpoint. Individuals were asked to rate health-related statements on a 7-point Likert scale, ranging from “totally disagree” to “totally agree”, with their level of agreement. Dimensions of the Lifestyle-HRSC include nutrition (8 items), social support (8 items), avoiding diabetes (10 items), physical activity (4 items), problem-solving (3 items), and challenges related to being healthy (3 items). Lifestyle-HRSC scores for each dimension were determined by calculating the average score for dimension-related items. The alpha reliability was 0.57 (pre-program) and 0.62 (post-program).
Weight and height measurements were obtained at baseline and endpoint by a trained research assistant. Height and weight were assessed using a portable scale (SECA 876) and stadiometer (SECA 213) to the nearest 0.1 kg and 0.1 cm, respectively. BMI was calculated by dividing weight (kg) by squared height (m). An objective measure of physical activity, steps and activity minutes, was captured using New Lifestyles-1000 pedometers at baseline and endpoint. Individuals were asked to wear the pedometer, either at the waist or on a belt or elastic band, for 7 consecutive days during all waking hours. Data were used if participants wore the pedometer for at least 4 days with 10 h of wear time/day [
28].
Data analysis: The Statistical Package for the Social Sciences (SPSS) was used for data analysis. Descriptive statistics were completed for sociodemographic information, outcomes (weight, BMI, steps per day, activity minutes per day), and predictors (Lifestyle-HRSC dimensions of nutrition, social support, avoiding diabetes, physical activity, problem-solving, and challenges related to being healthy). Two simple linear regression analyses were calculated to examine baseline and endpoint outcomes based on pre-program predictors.
2.3. Hybrid-Format DPP (Setting 2)
Participants: University employees between the ages of 18 and 64 years, with a BMI ≥ 25.0 kg/m2, and not diagnosed with type 2 diabetes, participated in the program. Eight individuals who completed the program were invited to attend a group interview. Three individuals who agreed to participate read and signed the consent form prior to attending the interview.
Procedure: The Hybrid-Format DPP followed the CDC-approved curriculum and was facilitated by two trained Lifestyle Coaches. The program occurred via Zoom (distance learning) for the first four months and a combination of Zoom/in-person during the final 8 months of the program. The format options and changes were in response to campus COVID-19 restrictions as well as participant comfort. DPP participants were invited to participate in a small, semi-structured group interview at the conclusion of the program. Interview questions were created to understand the participants’ experiences with the DPP as well as their thoughts on topics measured by the Lifestyle-HRSC, based on results from the Technology-Augmented DPP. A key intention of the interview was to identify features of the program that left an impact, positive or negative, on participants.
Data analysis: Qualitative data were analyzed by two undergraduate research assistants under the supervision of a co-author. The analysis team was not involved in National DPP implementation. A reflexive thematic analysis (RTA) was used following a step-by-step approach laid out by Braun and Clarke [
29]: (1) familiarization through review of transcription by two independent coders; (2) generating initial codes using NVivo qualitative analysis software version 12.0; (3) generating preliminary themes and subthemes; (4) reviewing themes for homogeneity between the codes within a theme and heterogeneity between overall themes; and (5) defining themes by ensuring all themes and subthemes contributed to a meaningful narrative in the context of the research goals. In practice, RTA is an iterative process. As such, the coders determined the appropriateness of themes by conducting a second pass over the transcript using the newly generated themes, revising codes and themes as needed. This process was repeated until themes were comprehensive representations of the data. Unlike coding reliability approaches, RTA does not assume an “accurate” way of coding data, and therefore inter-rater reliability was not assessed. Although consensus checks were conducted, the goal was not to achieve agreement of meaning but rather to sense-check ideas and discuss coder assumptions [
30]. A deductive approach was embraced as the goal of examining participant experiences with behavior change was informed by the Lifestyle-Health-Related Self-Concept (HRSC) questionnaire [
28].
3. Results
Results from the Technology-Augmented DPP appear in
Table 1 (demographic information),
Table 2 (descriptive statistics for measures), and
Table 3 (regression analysis). Results from the Hybrid-Format DPP appear in
Table 4 (themes and accompanying quotes).
3.1. Weight and BMI (Setting 1)
Lifestyle-HRSC dimensions (pre-program) related to baseline and endpoint weight in the Technology-Augmented DPP included social support [baseline F(1,46) = 6.55, p = 0.01, R2 = 0.13; endpoint F(1,46) = 9.94, p = 0.00, R2 = 0.18] and problem-solving [baseline F(1,46) = 5.20, p = 0.03, R2 = 0.10; endpoint F(1,46) = 9.45, p = 0.00, R2 = 0.17]. The avoiding diabetes dimension of the Lifestyle-HRSC was related to high weight at endpoint [F(1,46) = 4.38, p = 0.04, R2 = 0.09]. In relation to BMI, social support [F(1,46) = 6.60, p = 0.01, R2 = 0.13] and problem solving [F(1,46) = 10.27, p = 0.00, R2 = 0.18] were associated with high BMI at endpoint. Overall, at the beginning and end of the program, individuals with high weight and high BMI also perceived social support and problem solving to be important. At the end of the program, individuals with high weight perceived an emphasized importance of avoiding diabetes.
3.2. Activity Minutes and Steps per Day (Setting 1)
In the Technology-Augmented DPP, Lifestyle-HRSC dimensions (pre-program) were related to endpoint, not baseline, activity minutes. The dimensions related to endpoint activity minutes were nutrition [F(1,46) = 9.87, p = 0.00, R2 = 0.18] and problem solving [F(1,46) = 7.68, p = 0.01, R2 = 0.14]. For steps per day, dimensions were related to both baseline [nutrition F(1,46) = 4.85, p = 0.03, R2 = 0.10] and endpoint [social support F(1,46) = 5.52, p = 0.02, R2 = 0.11]. Overall, at the beginning of the program, individuals with low activity minutes and high steps per day perceived nutrition to be important. At the end of the program, individuals with low activity minutes and low steps per day perceived nutrition and social support to be important, respectively, while individuals with high activity minutes perceived problem solving to be important.
3.3. Participant Characteristics and Outcomes (Setting 2)
The Hybrid-Format DPP began with 13 participants (9 female, 4 male), and the average age was 46 (range 35–65 years). At baseline, the mean weight was 236.8 lbs. (SD = 79.4; range 152–457 lbs.), and the mean physical activity minutes was 204.7 (SD = 159; range 0–445 min). Eight participants completed the program (6 female, 2 male) and identified as White and Not Hispanic or Latino/a. In addition, all participants who completed the program completed an undergraduate degree. At endpoint, the mean weight was 271.3 lbs. (SD = 76.1; range 198–446 lbs.) and the mean physical activity minutes was 116.5 (SD = 90.5; range 0–280 min). The Hybrid-Format DPP participant baseline weight (236.8 compared to 199.1 lbs.) and physical activity (204.7 compared to 17.5 min) and endpoint weight (271.3 compared to 190.7 lbs.) and physical activity (116.5 compared to 45.3 min) were higher than in the Technology-Augmented DPP (setting 1) (see
Table 2).
3.4. Theme 1: Frequency Matters for Meaningful Engagement (Setting 2)
Those who participated in the group interview discussed barriers to success related to session frequency. Despite challenges fitting weekly sessions into their lives, participants experienced a loss of motivation when sessions started occurring monthly instead. One participant noted that they would “…hurry up and read it and write out a couple goals…” prior to the monthly session. Loss of motivation to be meaningfully engaged with the program may have been driven by a lack of accountability, as there were fewer touch points with the group to keep them on track. Moreover, as the program moved from weekly to monthly, attrition rates increased, which seemed to discourage some participants further.
3.5. Theme 2: Rules of Engagement (Setting 2)
Those who participated in the semi-structured group interview outlined several barriers to program engagement, leading to the generation of the theme Rules of Engagement. The overarching theme encompasses two sub-themes: Facilitation of Disclosure and Peer Support. Participants described how the lack of group participation stifled their ability to fully engage with the program. The lack of disclosure during group sessions was fueled, in part, by concerns of potential privacy breaches due to some online group members having their cameras off. Moreover, when participants were unable to see the body language and facial expressions of other members, they described feeling invalidated and unsure whether those members were even engaged in the conversation. Without assurances of privacy and equal engagement, participants felt uncomfortable openly sharing about their experiences. Participants also reported finding it challenging to know when to jump in and when to leave room for those online to share and desired greater involvement from the interventionist in facilitating communication between online and in-person group members.
Such barriers to disclosure hindered group participation and resulted in challenges harnessing the full benefits of the group format. The sub-theme of Peer Support was generated to reflect the discussions regarding the desire for more support from other group members. Participants reported benefitting from hearing the successes and real-life strategies being employed by other participants and noted that they would encourage each other to return to previous lessons and stay engaged. However, the gains from peer support were limited by the lack of overall group participation, and opportunities to support one another and hold each other accountable were missed.
3.6. Theme 3: Promoting Self-Efficacy (Setting 2)
The overarching theme of Promoting Self-Efficacy attempts to capture the central ideas underlying discussions of not feeling confident in reaching the goals of the program, despite finding the lessons useful. The first sub-theme, Applied Lessons, reflects desires for hands-on learning in addition to the lectures. One participant stated that the lesson topics were good, but that the canned stories often felt impersonal and unrealistic. On the other hand, having opportunities to practice exercises or cooking techniques could have increased their self-efficacy by teaching them concrete skills to use in their daily life. That is to say, despite being a skill-based program, those in the group interview lacked confidence in executing the skills they learned during the program.
The second sub-theme related to self-efficacy, Defining Success, was generated in response to frustrations regarding unsuccessful weight loss. Despite having successfully cut out unhealthy behaviors from their life, one participant stated that they did not feel successful due to not having lost weight. Another participant described feeling guilty that they did not meet weight loss goals, even though their blood work had improved. Small wins and success in domains other than weight were not adequately validated, thus impacting participant confidence in achieving program goals.
3.7. Theme 4: Bridging the Intention-Behavior Gap (Setting 2)
The theme Bridging the Intention-Behavior Gap was generated in response to participants struggling to articulate why they were unable to find the motivation to engage in the behaviors that were necessary to reach their goals. They described instances where they knew what they needed to do but were unable to “…make them want show up…” Participants seemed to be describing a disconnect with the extrinsic motivation that the program was tapping into. Extrinsic motivation is the desire to engage in a behavior due to an external pressure or reward (i.e., weight loss, improved health, program compliance) rather than personal enjoyment, so reliance on this kind of motivation is common within behavior change interventions [
31]. Although extrinsic motivation can be helpful at the beginning of a behavior change journey, it is often hard to sustain, as the motivation is dependent on the presence of external pressure or rewards that can lose their perceived value in the face of internal pressures such as discomfort when exercising or cravings for unhealthy food. Therefore, overreliance on extrinsic motivation may result in a widening of the intention-behavior gap and contribute to not reaching goals.
The second sub-theme identified within this theme was Leveraging Affect. Calls for the meaningful inclusion of affect in behavior change interventions and research have been issued in recent years [
32] as the growing body of research suggests that it can have a positive impact on behavior change [
33]. Discussions around feelings of guilt due to not achieving weight loss outcomes made apparent the opportunity to address negative affect during the intervention, particularly as it relates to self-efficacy concerns. One participant also implied that although it might be “…humiliating to stand on a scale in front of lead teachers…”, it may have strengthened their motivation to change their health-related behaviors to lose weight and avoid being humiliated. The participant was likely not endorsing this as a tactic that should be used, but the extract provides an example of how avoiding anticipated negative emotions can be intrinsically motivating.
4. Discussion
Based on our studies, the goals and structure of the National DPP may not meet the involvement and psychosocial support expectations and needs of rural participants, who are at greater risk of type 2 diabetes diagnosis [
19]. In both settings, participant experiences with the National DPP were associated with psychosocial factors known to be important for behavior change [
10,
15]. At the beginning of the Technology-Augmented DPP (setting 1), individuals with higher weight acknowledged the importance of social support and problem-solving strategies for risk reduction. Likely, this represents reasons for joining a group and skill-based prevention program. Though, Lifestyle-HRSC assessment also provided information about less than ideal health outcomes. Individuals who perceived social support, avoiding diabetes, and problem-solving skills as important at the start of the program also tended to have high weight and high BMI at the end of the program. Individuals who perceived social support and nutrition as important at the beginning of the program were also likely to have low steps and low activity minutes per day at the end of the program. Perceptions of the importance of social support, avoiding diabetes, problem-solving, and nutrition at the start may have affected program participation and resulting changes in health outcomes. That is, it is possible the individual needs and expectations were not met within the National DPP. Interestingly, the findings suggest there are different self-perceptions associated with different DPP outcome goals. Our studies emphasize the importance of examining ways to enhance and support the DPP [
28]. In the Hybrid-Format DPP (setting 2), participant discussions supported the research calling for greater promotion of self-efficacy [
31,
34], the inclusion of emotion-related intervention techniques [
33,
35], and changes in format to better support mixed-modality programs in enhancing group participation. Our findings support the continued need to learn about individual experiences and group preferences in order to support participant achievement of program outcome goals [
23].
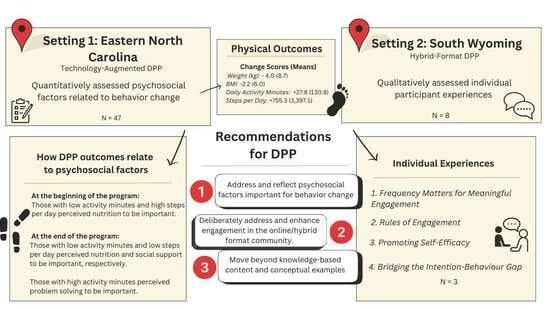
The studies’ results provide further insight into recommendations for National DPP implementation and research in rural settings. First, DPP program format content should address and reflect psychosocial factors important for behavior change. Motivation to engage in behavior change is impacted by factors such as emotional processes, self-efficacy, program engagement, and risk perception. The Lifestyle-HRSC found risk-reducing themes related to National DPP health outcomes were likely associated with perceptions of risk. The Lifestyle-HRSC may not specifically measure risk perception, but it may offer insight into the prevention behaviors that are viewed as most important (or not) to risk reduction. For example, an individual who perceives nutrition, physical activity, or social support as important may not have a realistic perception of their ability to reduce their risk. Therefore, the Lifestyle-HRSC might provide important insight into participant interactions with the program curriculum. The National DPP curriculum could include pre-sessions that understand and focus on risk perception related to specific lifestyle change topics [
36]. In addition, communication about diabetes risk prior to program attendance may influence individual perceptions [
37]. In the Technology-Augmented DPP, Lifestyle-HRSC questionnaire responses at the end of the program did not correspond to end-of-program outcomes. The National DPP sessions may not have changed participant perceptions of health that support positive health outcomes. While the National DPP does not intend to change perceptions of risk, behavior change is influenced by risk perception [
38]. In addition, the DPP should consider additional outcomes, other than weight loss. A focus on health behaviors, rather than weight, may encourage individuals to focus on health-promoting behaviors to prevent type 2 diabetes.
Second, DPP program sessions should deliberately address and enhance engagement in the online/hybrid format community [
39]. The didactic and content-focused nature of the National DPP may not effectively utilize group processes and interactions. Participants in the Hybrid-Format DPP provided notable insights into suggested changes to the programming, such as establishing rules for participant expectations and participation that could positively impact engagement, communication, and respect. Finally, post-COVID interventions, including virtual and mixed modality options, may require new and established guidelines for facilitator training (e.g., working with both online and in-person participants) and participant expectations (e.g., camera on). Specifically, results from the Hybrid-Format DPP study suggest the National DPP session format and implementation should be updated to reflect individual involvement needs that have changed since the COVID-19 pandemic [
40].
Third, DPP programs should move beyond knowledge-based content and conceptual examples. In the Hybrid-Format DPP, participants discussed frustration that the information-based nature of the sessions left little time for engagement and discussion with each other. Individual participation is important because engaged individuals are more likely to practice healthy behaviors, seek health information and sources, follow up with providers, and participate in self-monitoring [
41]. Findings from our study suggest that the National DPP may consider modifications to their curriculum to further improve type 2 diabetes prevention in at-risk populations. For example, individuals with higher weights, thus potentially at a higher risk of type 2 diabetes development than lower weight individuals, reported the importance of social support and problem-solving strategies. The National DPP curriculum should encourage within-group peer support and incorporate additional lessons focusing on social support. For instance, lessons can focus on identifying different types of social support for different behaviors (e.g., physical activity, nutrition, stress management) and give participants ample opportunity to share their personal experiences in each session. When presenting problem-solving strategies, some strategies may be beneficial to go beyond discussing healthy food choices and provide lessons on culinary and food preparation techniques to assist with food preparation self-efficacy. Many individuals understand the value of healthy eating but may not have the skills to adequately prepare healthy foods.
Strengths of our studies include the examination of two different National DPPs and the use of a new questionnaire created to examine strategies emphasized by the National DPP. In addition, both studies utilized a diverse sample of adults in work settings from rural areas. Limitations of the study should be considered when interpreting the results. First, regarding the use of the Lifestyle-HRSC, it is a newly developed questionnaire, and further study of the validity and reliability is needed. Second, while statistically significant relationships were found between the questionnaire and health outcomes, the analysis also revealed above-average to high agreement with most items as well as low variability in item responses. Our results may be an overestimation of the relationships between variables because individuals who choose to participate in a lifestyle change program would likely agree with the effectiveness of risk reduction. Third, our research examined the perceptions of individuals who completed the program, but understanding the perceptions of non-finishers is critical to identifying the factors that contribute to program success (or not). Individuals in both studies were from rural areas, and their experiences with the National DPP may only apply to others with similar experiences. Furthermore, there were only three participants from the Hybrid group who completed the focus group, thus limiting generalizability. Considerations of what constitutes a sufficient sample size are ongoing in qualitative research. Unlike quantitative research, there are few clear guidelines for determining a priori sample sizes or reaching data saturation, the point at which new codes or themes cease to emerge [
42]. Due to the specificity of our aim of understanding the individual experiences of those who completed the Hybrid-Format DPP and the richness of the data obtained, we were satisfied with reaching 37.5% of the completers. As stated previously, our results should be viewed in the context of DPP completers who were particularly motivated to engage in a post-intervention feedback interview. As such, we were unable to examine the barriers to engagement and behavior change that were endorsed by those who were least engaged in the program and potentially most at risk for attrition.
5. Conclusions
The National DPP is an important evidence-based prevention intervention, and the positive impact of the program on overall health outcomes is undeniable. However, the National DPP may only benefit certain individuals in specific circumstances and situations. It is especially important to further the research and implementation of the National DPP for the benefit of marginalized populations. Therefore, additional research of implementation in rural areas is essential. Based on our study, we believe a focus on understanding and responding to context-specific and participant-focused National DPP implementation is the essential next step in National DPP research. The Lifestyle-HRSC questionnaire revealed participant psychosocial support needs and may be used for translational research and practice in a variety of ways, including individual assessment and tailored program delivery. For example, a Lifestyle-HRSC assessment prior to program participation may offer information about individual strengths and deficits regarding lifestyle change activities. Future research should include assessment of psychosocial factors to further explain the findings of our research. In addition, updates to the National DPP session format and implementation might need an expanded focus on participant engagement, communication, and social support needs. Prevention programs and policies individualized to people and communities will improve participation and outcomes, and the National DPP should consider how to evolve to the changing needs of at-risk individuals.