1. Introduction
2. Patient and Methods
A 63-year-old Caucasian female patient was admitted for a diagnostic work-up due to an accidental finding of a right lung lesion on a chest X-ray. Although the patient did not experience any pulmonary symptoms (e.g., dyspnea, cough, or chest pain), she was a heavy smoker with a medical history of chronic obstructive pulmonary disease. A fibrobronchoscopy was performed, which revealed a large tumor infiltration of the bronchial mucosa in the bronchus of the right upper lung segment with complete obstruction of the right secondary bronchus. During this procedure, transbronchial needle aspiration and a biopsy were performed. A cytology specimen showed non-small malignant cells, possibly adenocarcinoma, and a histology specimen showed carcinoma of planocellular differentiation. The specimens were EGFR negative and PD-L1 positive (>90%). CT scans showed a lobulated lesion in the right upper lung segment measuring 39 × 29 × 37 mm, infiltrating some segments of pulmonary artery branches with a few satellite nodular lesions. There was no enlargement of the mediastinal lymph nodes, nor signs of disease dissemination. According to current guidelines, pathologic evaluation of mediastinal lymph nodes must be carried out—including mediastinoscopy, mediastinotomy, endobronchial ultrasound (EBUS), endoscopic ultrasound, and CT-guided biopsy—in order to exclude mediastinal involvement. Therefore, EBUS with transbronchial node biopsy was performed. The histology specimens were negative for malignancy. Fluorodeoxyglucose positron emission CT imaging revealed no signs of lymph node involvement or distant metastasis. The disease was staged as IIB (cT3N0), and the patient was presented to thoracic surgeons, according to whom the patient was medically inoperable due to poor pulmonary status. The multidisciplinary team decided to treat the patient using stereotactic ablative radiotherapy. Neither concurrent chemoradiotherapy nor immunotherapy was considered due to the poor pulmonary function. CT scans performed for simulation purposes showed enlargement of the intrapulmonary lesion, which measured 71 × 49 mm at that time. Our multidisciplinary team indicated PULSAR to treat the NSCLC using the adaptive Varian Ethos™ system.
To generate adapted plans using the Ethos system, an initial simulation and plan had to be made. This initial plan (also called a reference plan) was used as an optimization and contouring template for subsequent automatically generated online adapted plans.
Unlike online adapted plans, the generation of a reference plan normally takes significantly longer (several hours in this case) and thus could not be conducted online while the patient was waiting on the couch. Since the patient was treated in free breathing, a 4DCT was necessary to obtain information on the tumor respiratory movement needed for ITV volume definition. Initial planning CT images (free breathing, average, and 4DCT) were acquired using a Siemens Somatom Definition EDGE scanner.
Between all 10 phases of breathing, maximum lesion excursions did not exceed 3 mm, 5 mm, and 1 mm in the anterior-posterior, craniocaudal, and lateral directions, respectively.
Since a 4DCT could not be acquired during online adaptation, adapted planning was performed using a free-breathing CBCT, and a clinical target volume (CTV) structure was generated. Since HyperSight CBCT acquisition typically only lasts 6 s, it underestimates lesion respiratory movement and usually corresponds to an exhale breathing phase. Therefore, CTV to internal target volume (ITV) margins corresponding to 4DCT-detected maximal lesion excursions from the exhale phase (3 mm, 5 mm, and 1 mm in the anterior, caudal, and right direction, respectively) were added.
Finally, the ITV was expanded with an additional isotropic margin of 5 mm to generate a PTV.
The principal OARs were the lung, heart, tracheobronchial tree, and the first, second, and third right ribs. An adapted volumetric modulated arc therapy plan with three arcs and a total peripheral dose to the tumor of 36 Gy (D 50% = 45 Gy) in three fractions was generated using the Ethos treatment planning system (TPS) version 02.01.00 (Varian Medical Systems) and exported to Varian Eclipse TPS for the purposes of treatment comparison, as well as to the Mobius second-check dosimetry system for plan evaluation. Patient intrafraction motion was monitored using the AlignRT (VisionRT, London, UK) patient surface monitoring system. To optimize and calculate adapted plans, a HyperSightTM-acquired CBCT with iCBCT Acuros reconstruction was used. Each pulse was followed by a pause of four weeks, allowing for tumor response and reduction in volume.
After the pause, a new adapted plan was generated in the same manner, using CBCT images acquired while the patient was lying on the treatment couch waiting for the treatment.
3. Results
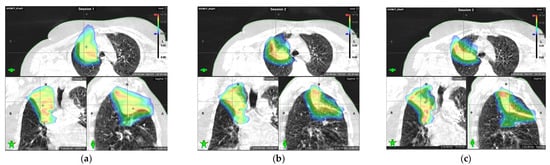
The reduction in target volume after the pulses (followed by pauses) resulted in a significant decrease in the dose to healthy tissue for all tissues except for the lungs. Due to tumor shrinkage, more lung tissue in the apical segment was exposed to a high dose when comparing the second and third pulse with the first one.
In addition, the patient had to travel to the hospital only for the initial CT simulation, since the others were carried out as a part of the online adaptation. This further accelerated and simplified the entire procedure.
4. Discussion
These findings are in accordance with previous PULSAR treatments delivered in our institution using the Varian Edge system. The change from Edge to Ethos adaptive systems reduced both the number and duration of patient stays at the hospital, as only the initial pulse requires a separate simulation CT and offline optimization process. Thus, the delay between planning CT acquisition and treatment delivery was reduced to a minimum. The whole duration of a pulse treatment, from the patient’s arrival to iCBCT acquisition, online plan adaptation, and treatment delivery, lasted no more than 65 min (47, 65, and 63 min for the first, second, and third pulse, respectively).
5. Conclusions
This report reinforces the previously stated concern that the treatment of large NSCLC in consecutive fractions without pauses and adaptations could result in overtreatment and increased toxicity compared with PULSAR. In addition, it demonstrates that an intelligent adaptive Ethos platform can reduce the number and duration of PULSAR patient stays at the hospital, as well as the time spent by staff (i.e., no need for separate additional CT simulations, as each new pulse is adapted based on an iCBCT acquired on the treatment couch). The Ethos intelligent adaptive system appears to be a promising platform for personalized treatments such as PULSAR.
Author Contributions
Conceptualization, D.S., D.K., B.J. and V.L.; methodology, D.S., D.K., B.J. and V.L.; validation, M.M., I.A. and H.K.; formal analysis, G.U., M.M. and I.A.; investigation, K.S. and A.A.; resources, M.M.; data curation, K.S., I.A. and A.Č.; writing—original draft preparation, V.L., B.J. and D.K.; writing—review and editing, A.A., M.M., H.K., G.U., K.S. and A.Č.; visualization, G.U.; supervision, D.S. and AA. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable to this study. This study was conducted in accordance with the local legislation and institutional requirements. The patient provided written informed consent for treatment and the publication of their anonymized data in this case study.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study, and written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
The data generated for this study are available in this article or from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. The study received no external funding.
References
- Sibolt, P.; Ottosson, W.; Sjöström, D.; Larsen, C.; Behrens, C.F. Adaptation requirements due to anatomical changes in free-breathing and deep-inspiration breath-hold for standard and dose-escalated radiotherapy of lung cancer patients. Acta Oncol. 2015, 54, 1453–1460. [Google Scholar] [CrossRef] [PubMed]
- Møller, D.S.; Holt, M.I.; Alber, M.; Tvilum, M.; Khalil, A.A.; Knap, M.M.; Hoffmann, L. Adaptive radiotherapy for advanced lung cancer ensures target coverage and decreases lung dose. Radiother. Oncol. 2016, 121, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Kwint, M.; Conijn, S.; Schaake, E.; Knegjens, J.; Rossi, M.; Remeijer, P.; Sonke, J.; Belderbos, J. Intra thoracic anatomical changes in lung cancer patients during the course of radiotherapy. Radiother. Oncol. 2014, 113, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Kavanaugh, J.; Hugo, G.; Robinson, C.G.; Roach, M.C. Anatomical adaptation—Early clinical evidence of benefit and future needs in lung cancer. Semin. Radiat. Oncol. 2019, 29, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Morris, Z.; Dohopolski, M.; Rahimi, A.; Timmerman, R. Future directions in the use of SABR for the treatment of oligometastatic cancers. Semin. Radiat. Oncol. 2021, 31, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.; Hsu, C.C.; Chen, W.M.; Chen, B.P.; Han, C.; Story, M.; Aguilera, T.; Pop, L.M.; Hannan, R.; Fu, Y.; et al. Personalized ultrafractionated stereotactic adaptive radiotherapy (PULSAR) in preclinical models enhances single-agent immune checkpoint blockade. Int. J. Radiat. Oncol. 2021, 110, 1306–1316. [Google Scholar] [CrossRef] [PubMed]
- Sezen, D.; Barsoumian, H.B.; He, K.; Hu, Y.; Wang, Q.; Abana, C.O.; Puebla-Osorio, N.; Hsu, E.Y.; Wasley, M.; Masrorpour, F.; et al. Pulsed radiotherapy to mitigate high tumor burden and generate immune memory. Front. Immunol. 2022, 13, 984318. [Google Scholar] [CrossRef] [PubMed]
- Aliru, M.L.; Zhang, Y.; Westover, K.D.; Timmerman, R.D.; Iyengar, P. Could poor outcomes for patients with limited lung function treated with SABR necessitate PULSAR? Int. J. Radiat. Oncol. 2023, 117, e1–e2. [Google Scholar] [CrossRef]
- Rahimian, J.; Bhattasali, O.; Girvigian, M.R. Adaptive dose-staged stereotactic ablative body radiotherapy for treatment of large central NSCLC lung tumors: A dosimetric simulation study. Int. J. Radiat. Oncol. 2023, 117, 709. [Google Scholar] [CrossRef]
- Tubin, S.; Vozenin, M.C.; Prezado, Y.; Durante, M.; Prise, K.; Lara, P.; Greco, C.; Massaccesi, M.; Guha, C.; Wu, X.; et al. Novel unconventional radiotherapy techniques: Current status and future perspectives—Report from the 2nd international radiation oncology online seminar. Clin. Transl. Radiat. Oncol. 2023, 40, 100605. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Lei, Y.; Wang, T.; Curran, W.J.; Liu, T.; Yang, X. Deep learning in medical image registration: A review. Phys. Med. Biol. 2020, 65, 20. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liang, X.; Shen, C.; Jiang, S.; Wang, J. Synthetic CT generation from CBCT images via deep learning. Med. Phys. 2020, 47, 1115–1125. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhu, X.; Hong, J.C.; Zheng, D. Artificial intelligence in radiotherapy treatment planning: Present and future. Technol. Cancer Res. Treat. 2019, 18, 153303381987392. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.F.; Witztum, A.; Valdes, G. Integration of AI and machine learning in radiotherapy QA. Front. Artif. Intell. 2020, 3, 577620. [Google Scholar] [CrossRef] [PubMed]
- Bogowicz, M.; Lustermans, D.; Taasti, V.T.; Hazelaar, C.; Verhaegen, F.; Fonseca, G.P.; van Elmpt, W. Evaluation of a cone-beam computed tomography system calibrated for accurate radiotherapy dose calculation. Phys. Imaging Radiat. Oncol. 2024, 29, 100566. [Google Scholar] [CrossRef] [PubMed]
- Sijtsema, N.D.; Penninkhof, J.J.; van de Schoot, A.J.; Kunnen, B.; Sluijter, J.H.; van de Pol, M.; Froklage, F.E.; Dirkx, M.L.; Petit, S.F. Dose calculation accuracy of a new high-performance ring-gantry CBCT imaging system for prostate and lung cancer patients. Radiother. Oncol. 2025, 202, 110596. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Park, Y.K.; Zhao, T.; Laugeman, E.; Zhao, X.N.; Hao, Y.; Chung, Y.; Lee, H. Image quality characterization of an ultra-high-speed kilovoltage cone-beam computed tomography imaging system on an O-ring linear accelerator. J. Appl. Clin. Med. Phys. 2024, 25, e14337. [Google Scholar] [CrossRef] [PubMed]
Comparison of dose distributions delivered during the first, second, and third pulses: (a) dose distribution delivered based on cone beam computed tomography (CBCT) images acquired during the first pulse; (b) dose distribution delivered based on the CBCT image acquired during the second pulse, four weeks after first pulse; (c) dose distribution delivered based on the CBCT image acquired during the third pulse, eight weeks after the first pulse. A substantial reduction in lesion size and dose to the surrounding tissue can be seen.
Figure 1.
Comparison of dose distributions delivered during the first, second, and third pulses: (a) dose distribution delivered based on cone beam computed tomography (CBCT) images acquired during the first pulse; (b) dose distribution delivered based on the CBCT image acquired during the second pulse, four weeks after first pulse; (c) dose distribution delivered based on the CBCT image acquired during the third pulse, eight weeks after the first pulse. A substantial reduction in lesion size and dose to the surrounding tissue can be seen.
Table 1.
Target structure volumes and organ at risk (OAR) volumes receiving one-third of the constraint doses (since the treatment was delivered in three pulses) compared between the pulses.
Table 1.
Target structure volumes and organ at risk (OAR) volumes receiving one-third of the constraint doses (since the treatment was delivered in three pulses) compared between the pulses.
| Target Structures, OAR Structures (Third of the Constraint Dose) | First Adapted Pulse (cm3) | Second Adapted Pulse (cm3) | Third Adapted Pulse (cm3) |
|---|---|---|---|
| ITV | 207.5 | 170.0 (−18%) | 149.6 (−28%) |
| PTV | 323.3 | 287.6 (−11%) | 275.7 (−15%) |
| Rib 1 (9.6 Gy) | 7.5 | 3.2 (−57%) | 4.2 (−44%) |
| Rib 2 (9.6 Gy) | 6.7 | 4.2 (−37%) | 4.6 (−31%) |
| Rib 3 (9.6 Gy) | 0.9 | 1.6 (+78%) | 2.3 (+156%) |
| Tracheobronchial tree (5.5 Gy) | 1.8 | 1.3 (−28%) | 1.2 (−33%) |
| Lungs (6.7 Gy) | 381.0 | 400.3 (+5%) | 425.9 (+12%) |
Table 2.
Maximum doses to organs at risk (OARs) (doses delivered to 0.1% volume of the organ) compared between three pulses.
Table 2.
Maximum doses to organs at risk (OARs) (doses delivered to 0.1% volume of the organ) compared between three pulses.
| Target Structures, OAR Structures (Third of the Constraint Dose) | First Adapted Pulse (Gy) | Second Adapted Pulse (Gy) | Third Adapted Pulse (Gy) |
|---|---|---|---|
| Aorta | 12.2 | 10.1 (−17%) | 10.7 (−12%) |
| Pulmonary artery | 14.2 | 13.1 (−8%) | 12.4 (−13%) |
| Tracheobronchial tree | 9.8 | 8.6 (−12%) | 8.5 (−9%) |
Table 3.
Time spent at each step of the treatment, from patient arrival to planning CBCT acquisition, through contour and plan generation, to plan delivery.
Table 3.
Time spent at each step of the treatment, from patient arrival to planning CBCT acquisition, through contour and plan generation, to plan delivery.
| Procedure Duration | |||
|---|---|---|---|
| Time Intervals | First Adapted Pulse (min) | Second Adapted Pulse (min) | Third Adapted Pulse (min) |
| From patient arrival to planning CBCT acquisition | 6 | 16 | 6 |
| From contour and plan generation to plan acceptance | 20 | 31 | 42 |
| First control CBCT and partial treatment delivery | 11 | 7 | 7 |
| Second control CBCT and the remaining treatment delivery | 10 | 11 | 8 |
| Total treatment time | 47 | 65 | 63 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Source link
Vanda Leipold www.mdpi.com