2.1.1. Allocation and Donor-Recipient Matching
The process of transplantation begins with the organ offer, and the decision to accept or reject the offered organ is of high importance. Since not all patients on the waiting list for KT would benefit satisfactorily from all donated kidneys, especially if the graft comes from an expanded criteria donor (ECD) [15], several decision-making tools have been developed to facilitate allocation and reduce discarded organs. The Kidney Donor Risk Index (KDRI), initially developed in 2009, combines 14 donor and transplant factors to predict the risk of graft failure after KT into a single number [16]. The researchers who developed the index concluded that transplants of kidneys with high KDRI (>1.45) are associated with decreased 5-year graft survival compared with the lowest KDRI quintiles. Subsequently, a variant of the KDRI was developed, named the Kidney Donor Profile Index (KDPI) [17]. The latter is based only on donor characteristics and is normalised to a percentile score. Organs with a KDPI ≥ 85%, also known as “high KDPI” organs, are associated with reduced 5-year survival and greater risk of graft failure compared to kidneys with KDPI < 85%.
To accomplish the best donor-recipient matching, an additional score was developed, namely the Estimated Post-Transplant Survival Score (EPTS). EPTS is a numerical measure combining four recipient parameters (candidate’s age and time on dialysis, current diagnosis of diabetes and prior solid organ transplants) in order to predict post-transplant survival and aid the allocation of donor kidneys [18]. Both KDPI and EPTS were implemented as part of the Kidney Allocation System (KAS) in 2014 by the United Network for Organ Sharing (UNOS) [19]. The current allocation system assigns priority to the top 20% of kidneys (as denoted by KDPI < 20) to patients with an EPTS of ≤20 [20]. Even though the use of the above scores provides an objective tool and their implementation may facilitate the identification of high-risk yet viable kidneys, there is a risk of adverse selection, paradoxically leading to excess organ discards. Bae et al. studied the discard rates before and after the implementation of KDPI. They reported no significant change in discard rate before (18.1%) and after KDPI (18.3%) among the entire population (adjusted odds ratio [aOR] = 0.97 1.041.10, p = 0.3). Nevertheless, among kidneys in which ECD and KDPI indicators were discordant, standard criteria donor (SCD) kidneys with KDPI > 85 were at increased risk of discard in the KDPI era (aOR = 1.07 1.421.89, p = 0.02) [21].
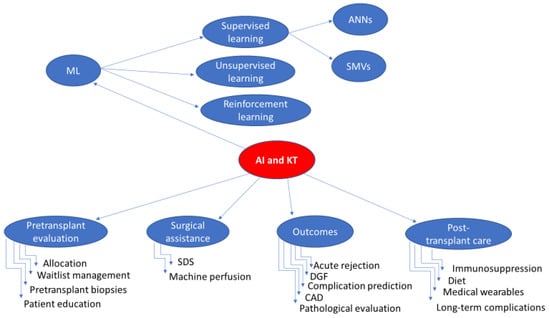
As the number of patients on dialysis increases and the number of organ donors remains limited, AI algorithms can be utilised to create a wiser allocation system. As stated already, AI algorithms have the ability to analyse large amounts of data. By considering factors such as blood type, tissue compatibility, donor-recipient age and medical history, AI can help identify the best matches and reduce the risk of rejection [6]. Furthermore, AI algorithms can assist in allocating organs more efficiently by analysing historical data and real-time information. This enables transplant centres to make data-driven decisions on how to allocate organs based on factors such as geographic distribution, transportation logistics and patient demographics [20]. Since the goal of smart donor-recipient matching is to maximise the functional lifespan of the donated organ, multiple studies have used ML algorithms to predict KT outcomes [22,23,24,25,26,27].
Bae et al. developed a prediction tool, available online, that estimates 5-year post-KT survival based on combinations of KDPI and EPTS scores using random forest algorithms. The researchers concluded that their model could support individualised decision-making on kidney offers in clinical practice [23]. In a different study, Brown et al. developed an ML Bayesian Belief Network, a form of graphical model that represents a set of variables and their conditional dependencies, functioning as a pretransplant organ-matching tool. Their model was able to predict graft failure within the first year or three years (sensitivity 40%; specificity 80%; area under the curve, AUC, 0.63) by analysing recipient body mass index (BMI), gender, race and donor age as parameters [24].
More recently, researchers developed an ANN model based on data from past organ donors, recipients and transplant outcomes in the United States and compared it with other survival analysis models. On the basis of the C-index, the ANN models had better discriminative ability than the Cox model and random survival forest model (0.650, 0.661 and 0.659 vs. 0.646 and 0.644, respectively). They concluded that their model could effectively predict KT survival and support optimal donor-recipient matching [27].
Kilambi et al. developed a decision-tree methodology to calculate the survival benefit of accepting a kidney vs. the survival benefit of rejecting it. Evaluating up to one year of future offers, the tool attains 61% accuracy. This methodology could help form personalised transplant decision-making [25].
Mark et al. combined different models to predict the 5-year post-transplant survival of KT recipients. Their proposed ML model, taking into account both donor and recipient characteristics, outperformed the EPTS (concordance index of 0.724 vs. 0.697), concluding that it has the potential to significantly improve the matching of organs to recipients [26].
Finally, Ali et al. developed a risk-stratification index using AI techniques. They used data from 156,749 Deceased-Donor KT between 2007 and 2021 from the UNOS database to train four ML models to predict death-censored graft survival. One of these models showed the best discriminative performance (area under the curve [AUC] = 0.66, 0.67, and 0.68 at 6, 9 and 12 years post-transplant), with time-dependent concordance (CTD) index at 0.66, outperforming the KDPI model (CTD: 0.59 and AUC: 0.60). They concluded that their models could aid decision-making in organ allocation [22].
Currently, AI-driven decision-making tools, including those mentioned earlier and others, are not yet fully integrated into formal kidney allocation guidelines. Instead, they are primarily used to supplement rather than replace human judgment.
2.1.3. Interpretation of Preoperative Grafts Biopsies
As stated before, the shortage of donor kidneys is a long-standing and intractable problem, but it is also exacerbated by a significant discard rate nearing 20% [30]. This high rate of discards is attributed in part to low utilisation rates of pretransplant graft biopsies for pathological assessment. Furthermore, improved electronic accessibility would be essential in addressing this matter [31,32]. Recent studies have demonstrated that AI and DL technologies can improve the effectiveness of pretransplant biopsies [33,34]. Marsh et al. developed a DL model to quantify glomerulosclerosis in kidney biopsy specimens, aiming to decrease the likelihood of unnecessary organ discards. Their model, capable of analysing multiple levels of a section, outperformed the capacity of pathologists, resulting in a 37% lower discard rate [35].
In another study, researchers developed a fully automated, DL-based algorithm called RENFAST (Rapid EvaluatioN of Fibrosis And vesselS Thickness) for the segmentation of kidney blood vessels and fibrosis in order to identify vascular and stromal injury of donors’ kidneys [36]. The authors reported that their proposed method showed excellent performance in both blood vessel and fibrosis segmentation (accuracy: 0.8936 and 0.9227, respectively), completing the task in a fraction of the time required by expert pathologists (2 min vs. 20 min per patient). The same authors also presented a second automated algorithm, called RENTAG (Robust EvaluatioN of Tubular Atrophy & Glomerulosclerosis), for the segmentation and classification of glomerular and tubular structures in biopsy specimens of donor kidneys. This algorithm also demonstrated excellent performance (dice score: 0.9529 for glomeruli and dice score: 0.9174 for tubule detection) and, as highlighted by the authors, could serve as a valuable tool to support pathologists’ diagnostic activities [37].
A recent systematic review concluded that existing AI algorithms in pre-implantation kidney biopsy pathology exhibited excellent and promising performance and underlined the significance of expert pathologist annotation to reliably train AI models [38].
Source link
Evgenia Kotsifa www.mdpi.com