1. Introduction
2. Materials and Methods
2.1. Study Design
All procedures were performed in a specialized laboratory with Xiscan 4400 Series Fluoroscopy from Fm Control/Group Alcor (Alava, Spain), which allowed detailed visualization during the procedures. The surgeons/study participants were divided into three groups according to their level of experience and familiarity with Minimal Incision Surgery (MIS).
This group consisted of 2 consultants who had attended training courses in minimally invasive surgery (MIS) but did not routinely practice these techniques in their daily clinical work. Their participation was crucial to assess the impact of customized surgical guidelines on professionals with theoretical training but no regular practical experience in these procedures.
This group consisted of 10 surgeons with limited experience in foot surgery. These professionals were in the early stages of their surgical career, with less than 5 years of experience performing minor surgeries and few procedures to correct hallux valgus. This group represented surgeons in training, whose skills were still developing.
This group included 10 surgeons with more than 15 years of surgical experience, specializing in foot surgery. These highly experienced professionals had a long history of performing complex procedures and served as a reference to evaluate how experience influences the performance of the surgical techniques studied.
To determine the existence of significant differences in the cut-off measures between three groups, a sample size calculation was performed using analysis of variance (ANOVA). Considering a significance level (α) of 0.05 and a test power (1-β) of 0.80, a large effect size (0.40) was established. The results indicated that 8 specimens per group would be required to ensure the detection of significant differences with these parameters. This setting allows working within the experimental limits while maintaining a reasonable probability of identifying relevant differences between groups.
2.2. Inclusion and Exclusion Criteria
To ensure the homogeneity and relevance of the results, strict inclusion criteria were established. Only cadaveric feet without significant structural deformities and with a length between 25.4 and 25.8 cm (equivalent to sizes 41–42 EU) were selected. These criteria made it possible to standardize the study conditions and minimize the variables that could affect the results.
Feet with previous deformities or injuries that could interfere with the accuracy of the osteotomies were excluded from the study. In addition, feet that did not comply with the established length measurements were discarded in order to maintain consistency in the sample conditions.
A total of 30 feet were selected, 10 in each group were included, although 2 of the feet in the 3d guise experimental group could not be evaluated due to the incorrect positioning of the surgical guide. There was a randomization of the samples that ensured that all groups had an equal opportunity to perform the procedures without specimen selection bias.
2.3. Surgical Technique
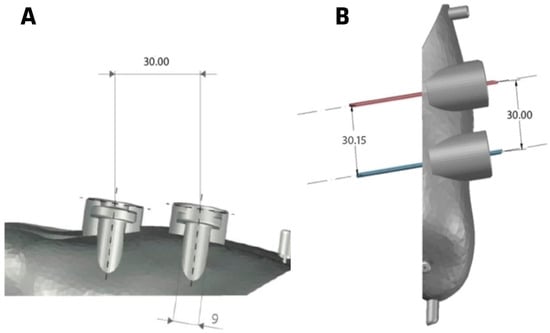
Surgeons in groups 1 and 2 performed a minimally invasive Reverdin-Isham procedure along with Akin Osteotomy to correct hallux valgus. All surgeons in both groups were given precise instructions to perform the osteotomies at a distance of 16 mm from the metatarsophalangeal joint line. For group 3, composed of non-MIS surgeons, a standard 3D-printed surgical guide was designed and fabricated. This guide, made of a single piece of 2-mm thick Polyamide 12, was adapted to the foot and covered the entire medial aspect of the first toe. The guide included two holes for fixation insertion using 2 mm K-wires and a 0.2 mm radiopaque element at 16 mm from the osteotomies for precise alignment with the joint line.
In this way all participants would try to perform the Reverdin and Akin osteotomies at 16 mm from the metatarsophalangeal joint line of the first toe.
2.3.1. Design Features of the Standard Surgical Guide
The standard surgical glove is 3D-printed to fit the first ray of the foot and is made from a single piece of polyamide 12, a material resistant to the high temperatures of an autoclave (125 °C–135 °C), ensuring its sterilization for intraoperative use. The material has a thickness of 2 mm, and at both cranial and caudal ends there are two holes for inserting Kirschner wires to secure the glove to the patient’s first ray. The guide covers the entire medial aspect of the first toe, extending from the proximal dialysis joint of the 1metatarsal to the most distal part of the toe, wrapping around both the dorsal and plantar sides of the first ray.
Fluoroscopic verification will confirm if the osteotomies are properly aligned with the anatomical landmarks of the first ray, as the aluminum wire should align with the interarticular line of the first metatarsophalangeal joint. The Akin and Reverdin osteotomies must be parallel to the metatarsophalangeal joint line and located 1.6 cm away from it.
Once the guides are verified to be correctly positioned using the fluoroscope, the glove is secured to the first ray with two Kirschner wires—one inserted at the most distal part and the other at the most proximal part. After completing the evaluation, positioning, and fixation of the glove, the next step is to perform the Akin and Reverdin osteotomies.
2.3.2. Operative Technique
The surgical procedure was the performance of the Reverdin-Isham technique which consists of making a precise longitudinal incision in the plantar-medial aspect of the foot, directly over the head of the first metatarsal. This incision is carefully deepened to reach the capsule of the first metatarsophalangeal joint, ensuring minimal disruption of the surrounding tissues. Once the capsule is exposed, a medium Shannon reamer is introduced through the incision. A wedge-shaped osteotomy is then performed, angled dorsally and distally toward the plantar and caudal aspects of the metaphyseal area of the metatarsal head. This angulation is crucial to achieve the desired correction while maintaining structural integrity. The technique must be executed with extreme care to preserve the lateral cortex.
After completing the osteotomy, the surgeon verifies its accuracy using a fluoroscope. Once the position is confirmed, the toe is gently rotated in abduction, which helps to compress and stabilize the Reverdin’s osteotomy site. The Akin osteotomy is then performed. This involves making an incomplete bony cut at the base of the first proximal phalanx, paying particular attention to preserving the lateral cortex. The Akin osteotomy also helps to correct the alignment of the finger.
For surgeons in the group using the 3D-printed surgical guide, the procedure was enhanced by attaching the guide to the first ray with the aid of a fluoroscope. The radiopaque line embedded in the guide was aligned with the joint line to ensure correct placement. The guide was then firmly attached to the first ray using two K-wires, one placed proximally and the other distally, providing stability for both the Reverdin and Akin osteotomies.
2.4. Radiographic Measurements
2.5. Statistical Analysis
All analyses were performed by an observer outside the experimental conditions. Data were expressed as mean and standard deviation (SD). Normality was assessed using the Shapiro–Wilk test. In addition, homogeneity of variance was calculated using Levene’s test. The significance level was set at p < 0.05. SPSS 24 (SPSS 24 Inc., Chicago, IL, USA) and Jeffreys’s Amazing Statistical Package (JASP)(0.18.3, Amsterdam, The Netherlands) were used to perform statistical treatment and the graphical representation of the data, respectively.
All analyses were performed using statistical analysis software (JASP, the Netherlands). The level of statistical significance was set at p < 0.05, implying that a statistically significant association would be considered when the p value was less than 0.05.
3. Results
For the measures Measure1 and Measure2, the 3D Guide group showed means of 15.10 (SD = 2.76) and 16.10 (SD = 2.83), respectively. The Master’s group obtained means of 12.03 (SD = 3.94) and 12.59 (SD = 3.67), while the Professionals group recorded means of 13.25 (SD = 2.62) and 13.56 (SD = 5.00). Although ANOVA analyses did not show statistically significant differences in either measure (Measure1: F = 2.05, p = 0.15; Measure2: F = 1.77, p = 0.19), the effect size in both cases was moderate (Measure1: η2 = 0.14, ω2 = 0.07; Measure2: η2 = 0.12, ω2 = 0.05), indicating that there were appreciable, though inconclusive, differences between the groups.
For Measure3 and Measure4, the differences between the groups were minimal. For Measure3, the 3D Guide group had a mean of 17.01 (SD = 2.78), while the Master’s and Professional groups had means of 15.45 (SD = 5.74) and 17.06 (SD = 5.57), respectively. ANOVA indicated F = 0.32 (p = 0.73) with a very small effect size (η2 = 0.02, ω2 = 0.00). Similarly, in Measure4, the means were 16.90 (SD = 3.30) for 3D Guide, 15.69 (SD = 6.53) for Master’s, and 15.68 (SD = 6.86) for Professionals, with ANOVA showing F = 0.12 (p = 0.89) and an equally small effect size (η2 = 0.01, ω2 = 0.00), suggesting high similarity between the groups in both measures.
Finally, for the angle measure, the 3D Guide group obtained a mean of 2.73 (SD = 0.36), while the Master’s and Professionals groups recorded much higher means: 14.27 (SD = 4.68) and 14.84 (SD = 9.07), respectively. ANOVA revealed a statistically significant difference (F = 10.66, p < 0.001), with a large effect size (η2 = 0.46, ω2 = 0.42), suggesting substantial and significant differences between the groups in this measure.
Although most of the measures did not show statistically significant differences, some (Measure1, Measure2) exhibited moderate effect sizes, indicating appreciable differences. However, the angle measure stood out due to its statistical significance and considerable effect size, suggesting clear and significant differences between the groups.
It can be observed that the 3D Guide group consistently exhibits lower dispersion across all measures, indicating greater consistency in its results. In contrast, the Professionals and Master’s students groups show greater variability, particularly in the Angle measure, where more pronounced differences between the groups are evident.
4. Discussion
The results of this study have clearly demonstrated that the use of 3D-printed surgical guides can significantly improve the precision of osteotomies in minimally invasive hallux valgus surgery. This study strongly validates the hypothesis that surgical guides not only reduce variability but also enhance accuracy in procedures performed by surgeons with varying levels of experience. The importance of these findings lies in the potential to standardize complex procedures, providing an additional tool to improve surgical outcomes.
The study does present several limitations and biases. First, the use of cadaveric feet may not fully reflect real surgical conditions, as they lack the dynamic factors present in living patients, such as biological responses to surgery and healing. Additionally, the sample size is limited, with only 28 cadaveric feet, which may affect the generalization of the results. There may also be variability in the skill level of novice surgeons, which could influence the results, although the use of surgical guides aims to minimize this factor. Lastly, the exclusion of feet with deformities may limit the applicability of the study to more complex cases.
5. Conclusions
The integration of 3D-printed surgical guides into minimally invasive hallux valgus surgery represents a significant advancement. These guides not only help standardize procedures and improve precision, but they can also accelerate the learning curve for novice surgeons, reduce surgical time, and minimize radiation exposure, thus improving both patient and professional safety. Future studies should focus on further optimizing guide designs and evaluating their effectiveness in a broader clinical context.
6. Patents
Drs. Ferrer-Torregrosa and Garcia-Vicente are inventors of the guiding patent and holding device for minimum-incision foot surgery (2014 PCT/ES2013/070877).
Author Contributions
Conceptualization, N.F.-E., E.N.-G. (Elena Nieto-González), C.B., S.G.-V. and J.F.-T.; data curation, J.F.-T.; Formal analysis, E.N.-G. (Eduardo Nieto-García), C.B., S.G.-V. and J.F.-T.; Investigation, N.F.-E., E.N.-G. (Eduardo Nieto-García), S.G.-V. and J.F.-T.; Methodology, N.F.-E., L.R.-A. and J.F.-T.; Project administration, J.F.-T.; Resources, S.G.-V. and J.F.-T.; Supervision, C.B. and S.G.-V.; Validation, N.F.-E., E.N.-G. (Elena Nieto-González) and J.F.-T.; Visualization, L.R.-A., C.B. and J.F.-T.; Writing—original draft, N.F.-E., E.N.-G. (Eduardo Nieto-García), L.R.-A., S.G.-V. and J.F.-T.; Writing—review & editing, N.F.-E., E.N.-G. (Eduardo Nieto-García), L.R.-A., E.N.-G. (Elena Nieto-González), S.G.-V. and J.F.-T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from the Centro de Investigación Traslacional San Alberto Magno (CITSAM).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. This research also complies with the guidelines and general principles included in the code of ethics of the General Council of the Spanish Association of Podiatrists, amended in 2018 (Código Deontológico|Consejo General de Colegios Oficiales de Podólogos (CGCOP). It also complies with Spanish Data Protection Legislation (L.O3/2018 of 5 December 2018).
Informed Consent Statement
All participants were informed prior to their inclusion in the project by means of a written consent form.
Data Availability Statement
Acknowledgments
The authors thank the Catholic University of Valencia San Vicente Maártir for their contributions and help in the payment of the Open Access publication fee.
Conflicts of Interest
None of the authors had any financial, personal, or professional conflicts of interest in relation to the results of this study.
References
- Brogan, K.; Lindisfarne, E.; Akehurst, H.; Farook, U.; Shrier, W.; Palmer, S. Minimally Invasive and Open Distal Chevron Osteotomy for Mild to Moderate Hallux Valgus. Foot Ankle Int. 2016, 37, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- de Prado, M. Complications in minimally invasive foot surgery. Fuß Sprunggelenk 2013, 11, 83–94. [Google Scholar] [CrossRef]
- Dhukaram, V.; Chapman, A.P.; Upadhyay, P.K. Minimally Invasive Forefoot Surgery: A Cadaveric Study. Foot Ankle Int. 2012, 33, 1139–1144. [Google Scholar] [CrossRef]
- Kaipel, M.; Reissig, L.; Albrecht, L.; Quadlbauer, S.; Klikovics, J.; Weninger, W.J. Risk of Damaging Anatomical Structures During Minimally Invasive Hallux Valgus Correction (Bösch Technique): An Anatomical Study. Foot Ankle Int. 2018, 39, 1355–1359. [Google Scholar] [CrossRef]
- Ferrer-Torregrosa, J.; Garcia-Vicente, S. Chapter Seven—Printed 3D in minimal incision surgery foot. In 3D Printing in Podiatric Medicine; Sandhu, K., Singh, S., Prakash, C., Subburaj, K., Ramakrishna, S., Eds.; Academic Press: Cambridge, MA, USA, 2023; pp. 139–149. [Google Scholar] [CrossRef]
- Calvo-Haro, J.A.; Pascau, J.; Mediavilla-Santos, L.; Sanz-Ruiz, P.; Sánchez-Pérez, C.; Vaquero-Martín, J.; Perez-Mañanes, R. Conceptual evolution of 3D printing in orthopedic surgery and traumatology: From “do it yourself” to “point of care manufacturing”. BMC Musculoskelet. Disord. 2021, 22, 1–10. [Google Scholar] [CrossRef]
- Ruiz-Romero, V.; Jorba-Garcia, A.; Camps-Font, O.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy of dynamic computer-assisted implant surgery in fully edentulous patients: An in vitro study. J. Dent. 2024, 149, 105290. [Google Scholar] [CrossRef]
- Petterson, A.; Kero, T.; Gillot, L.; Cannas, B.; Fäldt, J.; Söderberg, R.; Näsström, K. Accuracy of CAD/CAM-guided surgical template implant surgery on human cadavers: Part, I. J. Prosthet. Dent. 2010, 103, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Hopkins, W. A Scale of Magnitudes for Effect Statistics. 2002. Available online: http://www.sportsci.org/resource/stats/effectmag.html (accessed on 9 September 2021).
- Palmanovich, E.; Ohana, N.; Atzmon, R.; Slevin, O.; Brin, Y.; Feldman, V.; Segal, D. MICA: A Learning Curve. J. Foot Ankle Surg. 2020, 59, 781–783. [Google Scholar] [CrossRef]
- Krenn, S.; Albers, S.; Bock, P.; Mansfield, C.; Chraim, M.; Trnka, H.-J.J. Minimally Invasive Distal Metatarsal Metaphyseal Osteotomy of the Lesser Toes: Learning Curve. Foot Ankle Spec. 2018, 11, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Jowett, C.R.J.; Bedi, H.S. Preliminary Results and Learning Curve of the Minimally Invasive Chevron Akin Operation for Hallux Valgus. J. Foot Ankle Surg. 2017, 56, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Merc, M.; Fokter, S.K. IIS Learning curve in relation to radiation exposure, procedure duration and complications rate for Minimally Invasive Chevron Akin (MICA) osteotomy. BMC Musculoskelet. Disord. 2023, 24, 1–10. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.; Wang, M.; Jiang, Q.; Mo, A. Accuracy of Full-Guided and Half-Guided Surgical Templates in Anterior Immediate and Delayed Implantation: A Retrospective Study. Materials 2020, 14, 26. [Google Scholar] [CrossRef]
- Viet, H.; Thi Nhu Thao, D.; Phuoc, T.H.; Quang Tien, N. A multidisciplinary approach to managing severe gummy smile using 3D simulation and digital surgical guide: A case report. J. Surg. Case Rep. 2024, 2024, rjae483. [Google Scholar] [CrossRef]
- Brief, J.; Edinger, D.; Hassfeld, S.; Eggers, G. Accuracy of image-guided implantology. Clin. Oral. Implant. Res. 2005, 16, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Billings, A.; Scott, D.F.; Camargo, M.P.; Hofmann, A.A. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion: Long-term follow-up. J. Bone Jt. Surg.-Ser. A 2000, 82, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Evans, P.D.; Marshall, P.D.; McDonnell, B.; Richards, J.; Evans, E.J. Radiologic study of the accuracy of a tibial intramedullary cutting guide for knee arthroplasty. J. Arthroplast. 1995, 10, 43–46. [Google Scholar] [CrossRef]
- Duguay, T.; Housset, V.; Bouché, P.A.; Hardy, A.; Bauer, T. Prospective observational analysis of intraoperative radiation exposure with a mini C-arm intensifier in percutaneous forefoot surgery. Orthop. Traumatol. Surg. Res. 2023, 109, 103705. [Google Scholar] [CrossRef]
- van Rappard, J.R.M.; de Jong, T.; Hummel, W.A.; Ritt, M.J.P.F.; Mouës, C.M. Radiation Exposure to Surgeon and Assistant During Flat Panel Mini C-Arm Fluoroscopy in Hand and Wrist Surgical Procedures. J. Hand Surg. 2019, 44, 68.e1–68.e5. [Google Scholar] [CrossRef]
- Fernández-Vizcaino, C.; Nieto-García, E.; Fernández-Ehrling, N.; Ferrer-Torregrosa, J. Improving the Accuracy of Metatarsal Osteotomies in Minimally Invasive Foot Surgery Using a Digital Inclinometer: Preliminary Study. Sensors 2024, 24, 1022. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Vizcaino, C.; Naranjo-Ruiz, C.; Fernández-Ehrling, N.; García-Vicente, S.; Nieto-García, E.; Ferrer-Torregrosa, J. Impact of Minimally Invasive Intra-Capsular Metatarsal Osteotomy on Plantar Pressure Decrease: A Cross-Sectional Study. J. Clin. Med. 2024, 13, 2180. [Google Scholar] [CrossRef] [PubMed]
Surgical guide for group 3. (A) inferior vision, (B) superior vision.
Figure 1.
Surgical guide for group 3. (A) inferior vision, (B) superior vision.
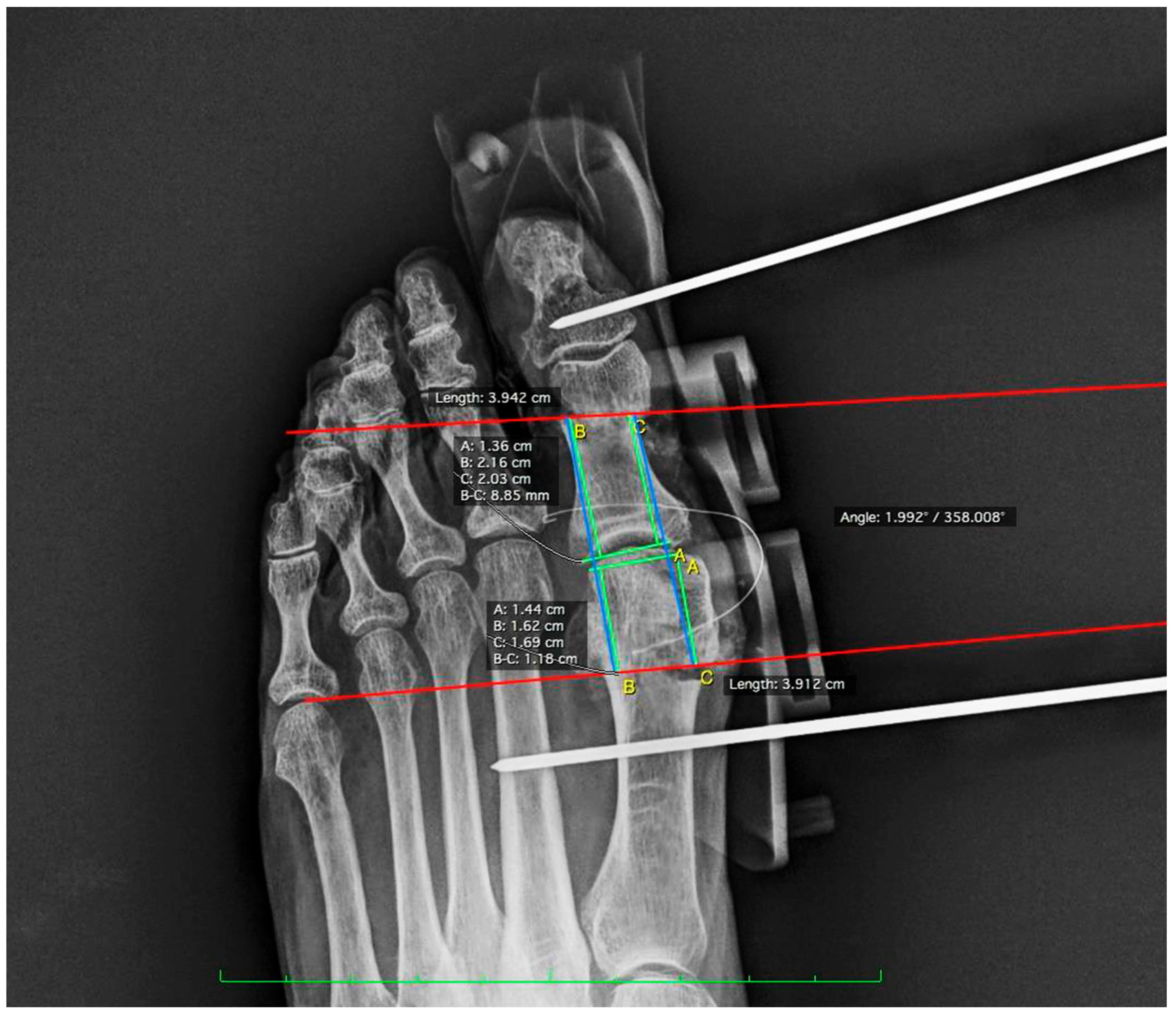
Post-surgical radiographic measurements lines using the Osirix program.
Figure 2.
Post-surgical radiographic measurements lines using the Osirix program.
Comparison of mean values and dispersion of the 3D Guide, Master’s, and Professionals Groups for all measures. The figure displays the median, interquartile range, and outliers for each group.
Figure 3.
Comparison of mean values and dispersion of the 3D Guide, Master’s, and Professionals Groups for all measures. The figure displays the median, interquartile range, and outliers for each group.
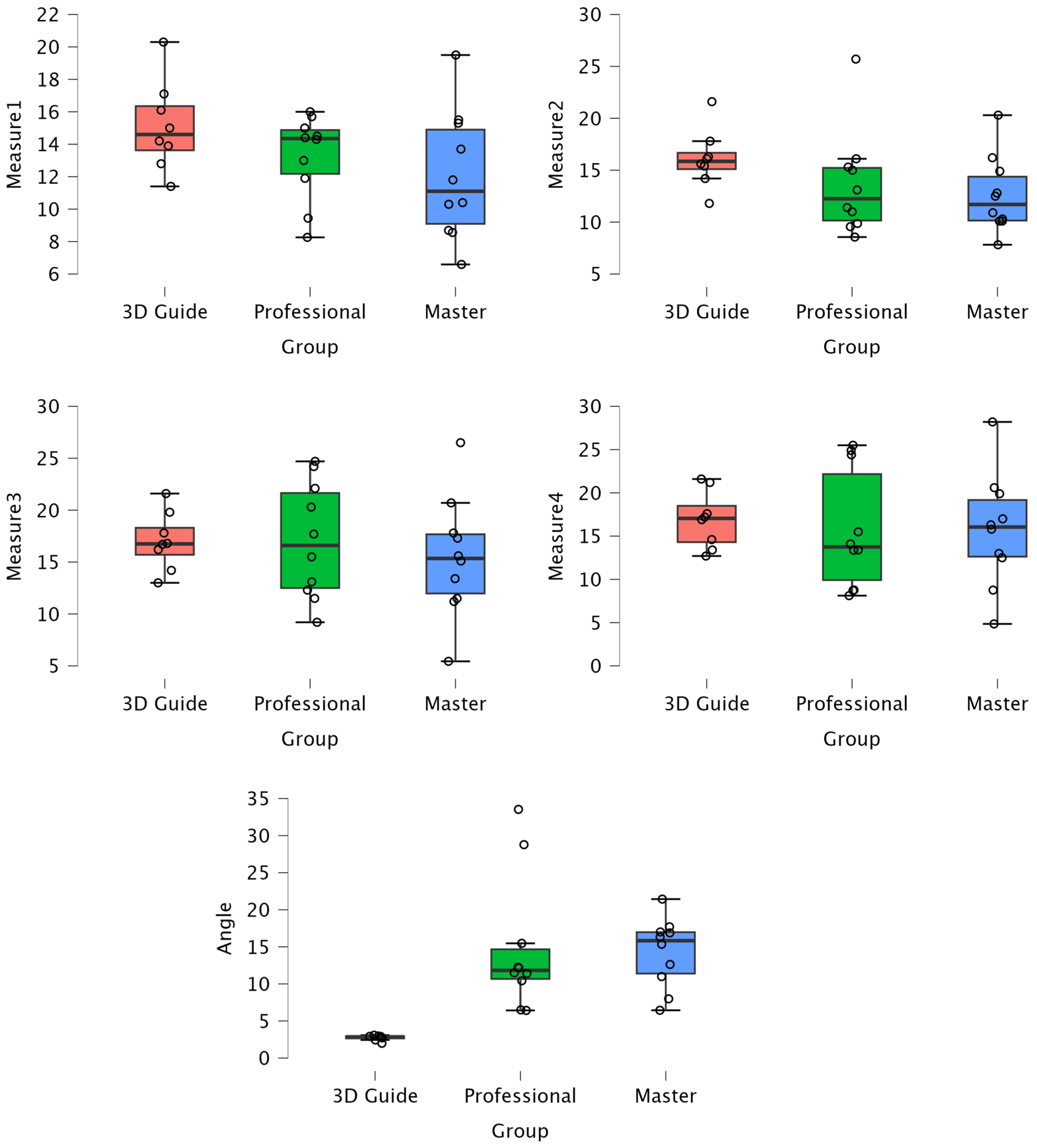
Table 1.
Comparison of descriptive statistics and significance analysis between groups for the variables studied.
Table 1.
Comparison of descriptive statistics and significance analysis between groups for the variables studied.
| Group | M1 | M2 | M3 | M4 | Angle | |
|---|---|---|---|---|---|---|
| 3D Guide | ||||||
| No. | 8 | 8 | 8 | 8 | 8 | |
| Mean | 15.10 | 16.10 | 17.01 | 16.90 | 2.73 | |
| S.D | 2.76 | 2.83 | 2.78 | 3.30 | 0.36 | |
| Minimum | 11.40 | 11.80 | 13.00 | 12.70 | 1.99 | |
| Maximum | 20.30 | 21.60 | 21.60 | 21.60 | 3.08 | |
| Master’s students | ||||||
| No. | 10 | 10 | 10 | 10 | 10 | |
| Mean | 12.03 | 12.59 | 15.45 | 15.69 | 14.27 | |
| S.D | 3.94 | 3.67 | 5.74 | 6.53 | 4.68 | |
| Minimum | 6.59 | 7.82 | 5.44 | 4.85 | 6.44 | |
| Maximum | 19.50 | 20.30 | 26.50 | 28.20 | 21.43 | |
| Professionals | ||||||
| No. | 10 | 10 | 10 | 10 | 10 | |
| Mean | 13.25 | 13.56 | 17.06 | 15.68 | 14.84 | |
| S.D | 2.62 | 5.00 | 5.57 | 6.86 | 9.07 | |
| Minimum | 8.26 | 8.56 | 9.20 | 8.12 | 6.42 | |
| Maximum | 16.00 | 25.70 | 24.70 | 25.50 | 33.53 | |
| Statistics | p-value | 0.15 | 0.19 | 0.73 | 0.89 | <0.001 a |
| η2 | 0.14 | 0.12 | 0.02 | 0.01 | 0.46 | |
| ω2 | 0.07 | 0.05 | 0.00 | 0.00 | 0.41 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Source link
Nadia Fernández-Ehrling www.mdpi.com