4. Discussion
Repercussions of the pandemic on liver transplant activity: The COVID-19 pandemic has repercussed on liver transplantation activity, with a decrease in the number of organ donors and even the temporary suspension of the activity in several centers [
3,
4]. A study which analyzed the database from the Global Observatory for Organ Donation and Transplantation between 2019 and 2020 observed a global decrease of 17.5% in the number of donors, with an 11.3% decrease in liver transplants [
28]. In an observational study which analyzed the transplant activity across 22 countries during the same period, a global decrease of 16% was observed [
5]; this decrease was more notable during the first months of the pandemic.
Inayat F et al. [
10] studied, retrospectively, a cohort of over 15,000 patients who received a liver transplant that were hospitalized between 2019 and 2020. They found that the COVID-19 pandemic did not translate into an increase in the risk of hospitalization in these patients. It was however shown to have an effect of increasing the intrahospital mortality and organ rejection rates among the patients hospitalized during said period.
In Spain, a study was conducted on organ donation among patients with a positive CRP for SARS-CoV-2 in 69 organ recipients who had negative CRPs. The CRP resulted positive in four of the recipients (5.8%) within 20 days of transplantation, without it being able to be attributed to the transplant. None among the 18 recipients of a liver transplant suffered major complications that could be linked to infection in the donor [
29]. Another multicenter study evaluated viral RNA in the liver biopsy of 10 grafts, with negative results being obtained in all of them [
30].
Characteristics of the transplanted patients: Kulkarni et al. conducted, in 2021, the only meta-analysis published to date [
1], including 18 observational studies with a total of 1522 patients. According to this study, the most common etiologies for transplant were viral (38%), alcohol (22.23%), NASH (2.5%), autoimmune (7.4%), and hepatocarcinoma (5.26%). In our study, viral liver disease, alcoholic liver disease, and hepatocellular carcinoma were the primary reasons for transplantation. The comorbidities that were most frequently registered were hypertension (44.3%), diabetes (39.4%), cardiovascular disease (16.43%), renal failure (13.7%), pulmonary disease (9%), and obesity (23.6%) [
9]. In our study, the frequencies of diabetes mellitus, hypertension, and obesity were similar, with frequencies of 41.07%, 38.93%, and 20.73%, respectively. The frequency of pulmonary disease (COPD or bronchial asthma) was 6.78%, while the frequency of cardiovascular events or a combination of multiple cardiovascular risk factors was up to 61.29%.
COVID-19 in orthotopic liver transplant: It was during the first wave of the disease that a large series of cases of adult liver transplant patients infected with COVID-19 were published, contributing greatly to the current knowledge of the particularities of the disease in this subgroup of patients [
8,
19,
20,
31,
32,
33].
The most common symptoms described in LT are fever (49.7%), cough (43.79%), and dyspnea (29.7%), with a 27.26% incidence rate of gastrointestinal symptoms [
9], myalgia or asthenia (36.66%), anosmia (36.66%), or dysgeusia (33.33%) [
7].
In our cohort, the predominant symptoms were not severe, with cough, asthenia, and myalgias encompassing the majority. Gastrointestinal symptoms (nausea, vomiting, and diarrhea) were only alluded to by 14.9% of patients. Among our patients, 25.5% referred to fever and 14.9% referred to dyspnea, with an observed progressive decrease in this latter symptom in the subsequent waves. Presenting at the time of diagnosis with asthenia, dyspnea, fever, or anorexia has proven to be a risk factor for developing respiratory insufficiency in this study, with dyspnea being the only symptom that proved to be a risk factor for the need of mechanical ventilation. The presence of fever and dyspnea were the only symptoms at the time of diagnosis that resulted in a higher risk of requiring intensive care.
The median time between receiving the transplant and COVID-19 diagnosis is variable, from 5.7 to 13.1 years [
7,
9,
34]. Guarino M et al. observed that it was significantly shorter in patients with asymptomatic COVID-19 [
2]. These, however, did not show any differences in regard to comorbidities or immunosuppressive treatment. In a 16-patient series, Eren-Kutsoylu et al. [
34] found a correlation between respiratory symptoms or fever and the need for hospitalization. In this series, 14 patients remained asymptomatic (46.67%), in contrast with the series by Colmenero et al., which included 7/111 patients who were asymptomatic (6.3%) [
8]. In this study, we found 19.87% of patients to be asymptomatic, with a variable frequency among different waves that was higher in the third and sixth (25.81–33.33%) versus the first and second (16.67–19.87%), all of which had a higher frequency than the last one (14.50%).
Kulkarni et al. describe a 72% rate of admissions, higher than in non-transplanted patients and three times higher than the one observed in our study, and a cumulative incidence of intensive care unit admission of 16%, compared to the 3.9% in our study [
9].
A mean hospital stay for LTRs of between 8 and 11 days was reported [
7,
32,
35], similar to that of the non-transplanted controls [
36] and shorter than that found in our study, which was 18 days. The incidence of invasive mechanical ventilation described in the above-mentioned meta-analysis was 21.1%, again higher in LTRs than in the non-transplanted controls [
9]. In our study, only five patients (1.63%) required intubation.
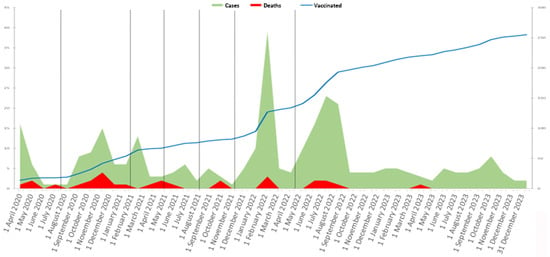
The lower rate of severe COVID-19 in this study is justified by the inclusion in the same of a higher number of patients towards the end of the pandemic. As can be observed in
Table 10, the rate of severe COVID-19 decreases towards the sixth and seventh waves, at which time over 60% of the cases were diagnosed. This draws attention, however, to the fact that the rate of intensive care unit admissions and the need for mechanical ventilation have shown no statistically significant differences during these periods.
In regard to thrombotic complications, the incidence among transplanted patients lies around 6% [
9]. Mansoor et al. [
20] found no differences when comparing this incidence rate to the thrombotic rate of the general public.
The median age at the time of diagnosis is lower (59.55 years) in transplanted patients compared to their controls (63.2 years). The median age at the time of diagnosis was similar in our study, 61 years. Colmenero et al. and Belli et al. describe that patients with less severe symptoms from COVID-19 were younger, had fewer comorbidities, and more frequently received immunosuppressive therapy with tacrolimus [
8,
19]. When compared to the general public, it can be seen that the course of the disease has not shown more severity in LTRs [
7,
33].
In this cohort, the median age and BMI were significantly higher in patients who suffered respiratory insufficiency or who required a longer hospital stay. In the logistic regression analysis, older patients and those who had a high BMI, renal failure with creatinine over 2 mg/dL, a history of cardiovascular events or risk factors, HTN, and T2D have been shown to be risk factors for respiratory insufficiency or hospital admission, while female sex proved to be a protective factor.
A history of COPD was a risk factor for hospital admission, as well as mTORi immunosuppressive therapy, while the number of vaccinations before diagnosis proved to be a protective factor for hospital admission and the development of respiratory insufficiency.
The time between vaccination and the start of symptoms was significantly shorter in patients who later developed respiratory insufficiency, but no significant differences were observed for hospital admission, admission in the ICU, or need for intubation.
Altered x-rays were observed to be a significant risk factor for severe COVID-19 (hospital admission, intensive care unit admission, respiratory insufficiency, or need for mechanical ventilation).
COVID-19-related mortality in orthotopic liver transplant: The factors related to death from COVID-19 have been exhaustively studied. The results for mortality in LT are heterogenous in the published series [
9], with a 16.5% incidence and similar values when compared to non-transplanted patients. Webb et al., in a multicenter study with 151 LTs among 18 countries, described a significantly lower mortality rate in LT (19% versus 27% in non-LT;
p = 0.046). The main causes of death that are described are COVID-19-related complications (62.54%) and respiratory failure (29.88%) [
8,
9,
19].
Increased levels of transaminases during COVID-19 infection have been documented [
9]. Rabiee et al. described an association between changes in hepatic biochemistry and increase in mortality in a series of 112 LTRs [
33]. Despite this, no differences were apparent in this study when analyzing alterations in hepatic biochemistry and death by COVID-19.
Concerning acute renal failure, a 33.22% incidence rate was reported in LTRs with COVID-19 [
9], indicating that the increase in basal serum creatinine concentration to be a risk factor for severe COVID-19 and mortality [
31,
36].
Other contributing factors to COVID-19 mortality are the presence of malignant extrahepatic neoplasia [
32], advanced age [
8,
19,
31], dyspnea at the time of diagnosis [
8], male sex, D-dimer or ferritin level elevation, and lymphopenia [
8,
32,
37].
In our study, the variables related to death by COVID-19 were obesity, renal failure, COPD, and DM2, while vaccination and immunosuppressive therapy with CNIs were protective factors. All the patients admitted to the ICU and those who required IMV were male as well as 10/12 (83.33%) of the patients who died from COVID-19.
Immunosuppression: The immunosuppression schemes in previously published studies are based on CNIs, cyclosporine, MMF, or mTORi in monotherapy or in combination [
8,
9,
19,
31,
32]. Colmenero et al. showed the prejudicial and dose-dependent effect of MMF immunosuppression [
8], possibly in relation to a synergic mechanism in cytotoxicity, on CD8+ with the COVID-19 virus. They did not find worse results in terms of severity in immunosuppressed patients with CNIs or mTORi. Belli et al. did prove an association between CNIs and reduced mortality which could be related to an inhibitory mechanism of viral replication [
19]. mTOR inhibitors, AZT, and MMF can induce cytopenia, which could worsen the course of infection since lymphopenia is a parameter associated with severe COVID-19 [
38,
39].
A change in immunosuppressive therapy has not been shown to have an impact on mortality [
19,
31,
34,
37,
40].
The consensus among the AASLD and the EASL is that an individualized evaluation of each case of COVID-19 infection, preferably reducing the dosage of mycophenolate in patients at a higher risk of developing severe forms of the disease, is ideal [
41,
42].
Vaccination against COVID-19: LTRs have shown a lower prevalence of anti-SARS-CoV-2 antibodies in the long term when compared to the general public, with higher levels of antibodies being seen in vaccinated patients [
43,
44,
45] and in patients with a longer period between receiving the transplant and being infected by COVID-19 [
43].
Currently, 12 vaccinations comprise the Emergency Use Listing of the WHO, including inactivated viral vaccines and protein-based and DNA or RNA viral vector-based vaccines [
46,
47]. The development and prompt distribution of the different vaccines has meant a change in the course of COVID-19, protecting against more severe forms and death. In LTRs, it has been proven to reduce the rates of infection, symptomatic disease [
11], hospitalization [
12], the need for intensive care and mechanical ventilation [
13], and mortality, particularly in patients with a complete course [
11,
12,
13]. The associations for the study of liver disease recommend a complete vaccination, as well as a booster dose to achieve or maintain immunity in LTRs [
48,
49]. This subgroup exhibits a lower immunological response than the general public due to receiving immunosuppressive therapy—particularly with MMF-—achieving a higher seroconversion dose in patients who received repeated doses [
44,
50,
51,
52]. Long-term LTRs show a better immunological response than recent recipients [
53].
This study shows a lower prevalence of severe COVID-19 in vaccinated patients, with a higher number of doses in those patients who did not present with complications.
Treatment for COVID-19 infection in LTRs: Together with general measures such as hand washing, the use of facemasks, and social distancing, multiple drugs have been evaluated as potential treatments for COVID-19, including hydroxychloroquine, antibiotics, antivirals, steroids, immunomodulators, anticoagulants, and plasma [
9].
Antimalarials such as hydroxychloroquine were considered during the first stages of the pandemic for their immunomodulator and antiviral effects, but their efficacy has not been clearly proven [
17,
54]. Remdervir, a SARS-CoV-2 RNA polimerase inhibitor, has been widely used since it is a medication with an acceptable safety level, but it has not shown strong benefits in patients with a solid organ transplant [
55,
56], which induced the WHO to discontinue its use in hospitalized patients [
55]. Nonetheless, it is still recommended for outpatient treatment in those with a high risk of hospitalization [
57]. Favipiravir [
58] and Lopinavir/Ritonavir, which showed in vitro activity against SARS-CoV-2 [
54,
59], are discouraged. Dexamethasone has proved to reduce mortality in those who require mechanical ventilation [
60]. Tocilizumab, an IL-6 receptor inhibitor, is considered a safe medication in transplanted patients, even though it must be used carefully owing to its hepatotoxicity [
54,
59]. Other monoclonal antibodies such as bamlanivimab, casirivimab, and imdevimab have proven to reduce the viral load in patients with non-severe COVID-19 [
55].
In our study, we observed that antimalarials, interferon, and kaletra were used during the first period in selected cases. When bacterial superinfection was suspected, empiric antibiotics were prescribed and later switched according to antibiogram. There was no immunosuppressive adjustment depending on the antibiotic administration, but all the patients had repeated immunosuppression level controls to maintain appropriate dosing during their hospitalization. Prophylactic anticoagulation was prescribed in 50% of the patients up to the fifth wave, with a decrease in the last two waves, following the same tendency as corticoid treatment.
Tocilizumab and remdesivir were used in 2.61% (N = 8) and 8.79% (N = 27) of the patients, respectively. The use of Paxlovid requires careful monitoring in immunosuppressive therapy; therefore, its use is limited in transplant patients [
61]. In our study, it has only been used in 1.02% of patients (N = 3).
Study limitations: This study has limitations due to its observational and retrospective design. Data were missing, as their report in the electronic medical records was not routinely and prospectively collected for research, which led to the exclusion of potential study subjects. Recall bias may have occurred, as participants may inaccurately remember their experiences, as they were surveyed after the infection, with the exception of those admitted to the hospital. Despite collecting data from a considerable number of patients, this study evaluates a cohort in a single center, which limits its external validity and implies a selection bias.