1. Introduction
Idiopathic normal-pressure hydrocephalus (iNPH) is characterized by ventricular dilatation due to a disturbance in cerebrospinal fluid dynamics, excessive cerebrospinal fluid (CSF) accumulation, and normal intracranial pressure [
1]. Clinical signs of iNPH are characterized as a triad [
2]: (i) slow and progressive gait and balance deficits, (ii) cognitive decline, and (iii) urinary incontinence [
3]. The treatment of iNPH involves a ventriculoperitoneal shunt [
4,
5,
6,
7,
8]. The present study aims to fill the gap in the information collected during the infusion and tap test [
9,
10,
11]. Until now, only a walking test has been performed to evaluate clinical improvement in patients with suspected normal-pressure hydrocephalus and to select individuals who may benefit from a ventriculoperitoneal shunt. The patient’s neuropsychological status (cognitive decline is one-third of the triad symptoms [
12,
13,
14]) is unfortunately not assessed. It is generally held that better methods for the identification of responders and non-responders are needed. To date, cognitive status has been addressed only before or after the tap test [
15,
16,
17]. Pre- and post-tap test cognitive assessments [
18] showed, for instance, that a 5-point increase in MOCA scores is matched by an improvement in cognitive domains; an MMSE increase of at least three points can be considered a positive predictor for a shunt intervention [
17]; and an amelioration between 30 and 60 min after the tap test can be found in identical forms, Bingley’s memory test, and the reaction time test [
15]. Improvements in several tests were also reported after shunt surgery, highlighting the predictive value of cognitive assessment [
16]. Undoubtedly, pre- and post-tap test cognitive assessments remain a standard source of information; however, the procedure could also be improved by adding complementary data on the patient’s cognitive status. Studies have attempted to predict cognitive improvement post-ventriculoperitoneal shunt solely based on pre- or post-tap testing cognitive scores. If it is proven feasible, the intra-tap test cognitive assessment—occurring when pressure is manipulated—could, in principle, be a direct measure for predicting cognitive changes post-ventriculoperitoneal shunt. In the present study, we addressed patients’ cognitive performance during the procedure, in order to assess the feasibility of ultra-fast neuropsychological testing during CSF pressure modification. Based on our experience with Real-Time Neuropsychological Testing (RTNT) in awake surgery [
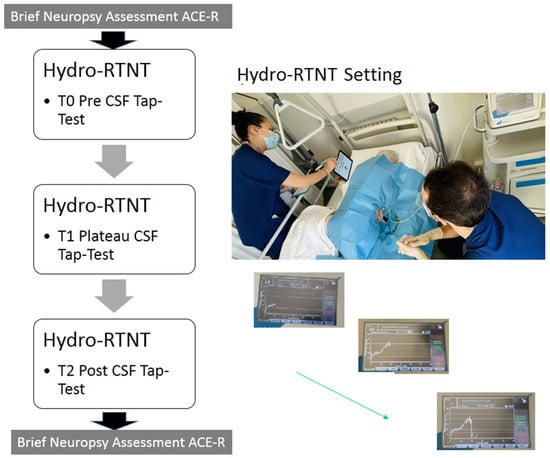
19], we performed a Hydro-RTNT in an iNPH setting. The neuropsychological protocol was administered at the patient’s bedside, immediately before the infusion test (T0), when a stable pressure plateau was reached (T1), and immediately after CSF subtraction at the end of the tap test (T2). We hypothesized that fluctuations in cognitive performance between T0 and T1 (at the end of the infusion phase, when the intracranial pressure was maximal) would indicate that changes can be observed in real time in patients with iNPH owing to the increase in intracranial pressure. Thus, the cognitive aspect may become a relevant evaluation index in future tap test responders. Furthermore, possible fluctuations in cognitive performance between T0 and T2 (after CSF subtraction, when the intracranial pressure reached values near 0 mmHg) would suggest that there may be improvements due to CSF drainage during the tap test.
4. Discussion
Based on our experience with RTNT in awake surgery, we tried to evaluate neuropsychological modifications, if any, during the infusion and tap test. The Hydro-RTNT approach differs from neuropsychological testing reported in the literature on iNPH patients (e.g., [
15,
16,
17]) because it is an intra-procedure monitoring technique. In particular, neurocognitive assessment was used in previous studies only before or after the tap test [
15,
16,
17]. Previous studies were aimed at detecting good predictors for a shunt intervention among test scores [
17]. Here, we set out to assess the feasibility of an intra-procedure assessment. However, future studies are needed to establish whether the Hydro-RTNT test scores could serve as good predictors for a shunt intervention, also including the collection of post-shunt intervention data (which are missing in the present study). We believe the study goal was reached as we showed that fluctuations in cognitive performance could be detected at the end of the infusion phase and after CSF was removed. Fluctuations were not generalized, as they were selective for some of the tests administered. These tests were tests tapping executive functions, namely the backward counting task [
23] and the verbal fluency task [
25].
In addition, while previous studies showed cognitive amelioration between 30 and 60 min after the tap test [
15], suggesting that testing carried out after the lumbar tap would provide much more reliable prognostic information, we showed that fluctuations in cognitive performance occur even earlier. We nonetheless acknowledge that, while the cortex mapping can quickly be performed during awake surgery for glioma, here, the cognitive improvement usually appears slowly after improvement of the intermittent intracranial hypertension.
We found that the reverse effect index was higher (i.e., high scores indicate a difference between backward and forward counting time, thus providing a measure of the iNPH patient’s executive abilities) at T0 vs. T1 and at T0 vs. T2. To interpret the reverse effect index, we looked at the time of completion and found that the reverse effect index at the plateau decreased because the time of completion for counting forward increased at the plateau. Patients were slower at counting forward at T1 vs. T2, indicating a worsening until a stable pressure plateau was reached, as compared to post-CSF drainage until pressure reached a value of 0 mmHg. Patients were slower at counting backward at T1 vs. T2, indicating a worsening after CSF drainage, as compared to a stable pressure plateau. Furthermore, they were slower at T0 than T2. Our results complement Kanno et al.’s [
23] study showing that the backward counting task is useful for evaluating executive dysfunction in iNPH and show that this occurs also when the backward counting task is administered during the procedure. Authors argue that changes in the reverse effect index show the severity of executive dysfunction.
Second, we found that verbal fluency performance—it being a measure of executive functions, too—changed during the CSF tap test. We found a worsening at T1 (vs. T0) and at T2 (vs. T0). We ruled out the possibility that such a pattern was related to verbal frequency, as the key letter was randomized every time. We did not observe an improvement at T2; this raises the question of whether the T2 assessment was carried out at a proper time in order to observe significant changes. We performed the T2 testing right after the CSF drainage; however, clinical status and gait were evaluated later, 24h after the procedure. In future studies, we will address this issue by changing the timing of the Hydro-RTNT design. A re-evaluation of RTNT patients after 24 h could bypass the clinical condition of discomfort experienced by some patients at the end of the procedure, such as headache or an uncomfortable position (fully lying down). These aspects may have interfered with the levels of attention and concentration during task administration.
Some authors [
30] studied the improvement in executive functions after shunt intervention in patients with NPH. Patients were administered tests tapping naming, short-term memory, attention, and fluency before and after the intervention and showed significant improvements. This shows that patients with NPH who respond positively to slow and continuous drainage of lumbar cerebrospinal fluid following ventriculoperitoneal shunting improve their performance on executive function tasks. Other authors [
31], using the Computerized General Neuropsychological INPH Test (CoGNIT) on 41 patients, found an improvement after shunt in all cognitive domains assessed before surgery. Patients improved in memory, executive functions (Stroop test), attention, psychomotor speed, and manual dexterity. Overall, the observed pattern of performance on backward counting and verbal fluency tasks indicates that changes can be observed in real time in patients with iNPH due to CSF infusion. We thus suggest that the cognitive aspect may become a relevant index to consider in future infusion and tap tests. Such indices could be very informative, as it is known that even cognitive changes, if untreated, may likely become irreversible due to the pathogenesis of iNPH [
32,
33].
A third result concerns the difference in patients’ performance on the brief neuropsychological assessment, with ACE-R used pre- and post-procedure. This assessment is carried out at the patient’s bedside when the patient can be brought to a 45–90° position to facilitate both concentration and the administration of the copying and writing subtests. We found that patients obtaining an ES of 1 pre-procedure—1 indicating a borderline performance—obtained an ES of 2 indicating normal performance post-procedure. A consistent number of them showed this trend (12.28% pre-procedure to 24.56% post-procedure).
This might suggest that in patients with borderline performance, CSF removal leads to an improvement in performance, shifting it fully to normal. Subtests contributing raw scores to improvement include phonological and semantic fluency tests as well as memory tests, in line with what has been reported for domains most affected in patients with iNPH. This aspect is less evident in patients with pre-procedure performance largely in the normal range. However, it may be useful in the future to re-evaluate patients a few days after deliquoration to measure the long-term effectiveness of the procedure.
In general, we acknowledge that patients’ performances were quite inhomogeneous during evaluations; this was confirmed by the high standard deviations calculated for each task. In future studies with larger samples, it could be possible to stratify patients according to their initial pre-procedure brief neuropsychological assessment and test how they perform at the Hydro-RTNT.
This is a pilot study conducted to assess the feasibility of Hydro-RTNT in patients undergoing a tap test. In the future, the Hydro-RTNT could help surgeons to identify good responders to shunting producing positive motor effects, without causing negative cognitive and/or emotional changes. Such alterations, if not revealed in real time during the tap test, would likely be observed as post-surgical outcomes. We are planning to carry out a larger multicenter prospective study to demonstrate the role of neuropsychological modifications in iNPH patients. The Hydro-RTNT protocol could be easily adapted to different patients’ populations; parallel forms of tests can be assembled by neuropsychologists, using the standardized and normed tests for other populations.
Limitations
This was the first study using a new, ultra-fast, and easy neuropsychological testing method for infusion and tap tests in patients with possible and probable iNPH. We acknowledge that our sample size is limited and could therefore limit the generalizability of the results. On the other hand, we used stringent inclusion and exclusion criteria in patients’ selection, and this could have reduced our eligible sample.
We also acknowledge that the postures used during this test may have influenced the effectiveness of cognitive tests. However, the neuropsychologist always ascertained that the patient could perform the test.
False positives and false negatives cannot be fully excluded, even when strategies to improve testing accuracy are used. Patients’ scores were evaluated in consideration of comprehensive clinical information collected from them. Performance was always evaluated as a relative change between serial neuropsychological testing, and not as single scores. We certainly need to identify better strategies to cope with false positives and false negatives when classifying single patients as good or bad responders in future studies.
Another limitation is that neuropsychological testing data after VPS implant are not presented, because the follow-up is still ongoing. For this reason, we cannot compare results at different times of follow-up. We are aware that the usefulness of the Hydro-RTNT approach can only be evaluated by testing putative correlations between intra-procedure and post-shunt data. This correlation analysis will also enable us to determine whether the Hydro-RTNT approach carries the same predictive power as currently established post-lumbar puncture tests. Finally, we assessed cognitive functions at the end of the tap test, but we cannot test patients after 12–24 h for logistic reasons. This is a problem that needs to be corrected in the future.