1. Introduction
Enterobacteriaceae comprise 50% of clinical isolates in healthcare-associated infections (HAIs), and 80% are Gram-negative bacteria. Within the Enterobacteriaceae, the genus
Klebsiella spp. is the second most important, and
Klebsiella pneumoniae is the most prevalent species with the most significant clinical relevance [
1].
K. pneumoniae is the cause of a substantial proportion of HAIs (30%), which includes soft tissue infections, urinary tract infections, pneumonia, and sepsis [
2]. Due to multiple pathogenicity factors, such as adhesins and capsule formation, that act as an antiphagocytic factor,
K. pneumoniae is considered an intrinsically pathogenic bacterium [
3].
K. pneumoniae belongs to the group of bacteria called ESKAPE, which refers to six bacteria responsible for most nosocomial infections that “escape” the effects of antimicrobials and includes
Enterococcus faecium,
Staphylococcus aureus,
K. pneumoniae,
Acinetobacter baumannii,
Pseudomonas aeruginosa, and
Enterobacter spp. [
3,
4]. In-hospital strains of
K. pneumoniae reach high levels of resistance to antimicrobials, reaching 61.4% of strains with multidrug resistance (MDR), 22% of strains with widespread antimicrobial resistance (XDR), and 1.8% of strains pan-resistant to all antimicrobials (PDR) [
5]. All
K. pneumoniae strains present natural resistance to ampicillin encoded, for example, in the BlaTEM-1, and many clinical isolates are producers of extended-spectrum beta-lactamases (ESBL) [
6]. XDR bacteria may also produce carbapenemases, β-lactamases that hydrolyze penicillins, cephalosporins, carbapenems, and monobactams [
7].
Carbapenamase-producing strains represent a severe risk since they are associated with infections with high morbidity and mortality, especially in patients with prolonged stays in the ICU or exposed to invasive devices [
8,
9]. These strains show resistance to all beta-lactams (penicillins, cephalosporins, monobactams, and generally intermediate resistance to carbapenems), so effective antimicrobial options are often lacking, and treatment depends typically on more toxic drugs such as aminoglycosides and polymyxins [
10]. Strains resistant to polymyxin, such as colistin, are increasing and represent an alarming proportion of isolates in some health centers associated with higher mortality [
7]. On the other hand, they have a large dissemination capacity because ESBL-type resistance is mediated by plasmids encoded in the bla
kpc gene [
11]. Dissemination via plasmids is much faster, as evidenced by the fact that practically 70% of the strains collected by the US CDC, as well as in Greece, Israel, Norway, Brazil, and Argentina, are the exact clone, ST258, the hyper-epidemic clone of
Klebsiella pneumoniae producing Bla
KPC-2 [
11]. Therefore, the antibiotics currently used are often ineffective in treating infections caused by multidrug-resistant bacteria. Consequently, developing non-antibiotic antimicrobial therapeutic alternatives is necessary [
12]. Several new strategies have been developed, such as using metallic nanoparticles, cationic polymers, peptidoglycans, nanocarriers, photo thermotherapy, and photodynamic therapy [
13]. Cationic compounds have been particularly widely used as PSs since they can weaken the permeability barrier of the outer membrane, allowing photosensitizer penetration [
14].
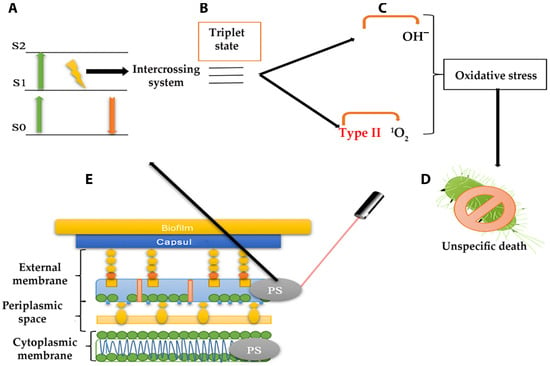
Antimicrobial Photodynamic therapy (aPDT) has demonstrated a substantial antimicrobial potential among therapeutic alternatives. APDT, used against cancer cells and microorganisms, uses photosensitizer (PS) molecules activated by light, causing local oxidative stress [
15]. It has also been used to treat various contaminations and for disinfection purposes, such as disinfection of water, blood, surfaces (hospitals), and medical devices, as well as food and crops [
16]. As shown in
Figure 1, PSs are non-toxic molecules that absorb energy at a specific wavelength (
Figure 1A) and transfer it to molecular oxygen in biological solutions (
Figure 1B) [
13]. The activation of oxygen produces reactive oxygen species (ROS), such as superoxide (O
2•−), hydrogen peroxide (H
2O
2), hydroxyl radicals (
•OH), and singlet oxygen (
1O
2) (
Figure 1C). ROS causes bacterial cell death by oxidizing organic macromolecules that are part of the cell envelope, such as lipids and proteins, or in the cytoplasm, such as nucleic acids. Bacterial cell death is unspecific because it destroys structures such as the plasma membrane, cell wall, and bacterial genome and can also distress vital processes by affecting enzymes and ribosomes (
Figure 1D) [
17]. The generation of ROS will be effective, depending on the photochemical characteristics of the photosensitizer; for example, a longer lifetime in excited states is essential to improve the probability of interacting with triple oxygen [
18,
19,
20]. PS can be administered systemically intravenously into the bloodstream or applied locally as a topical to the skin [
15]. Once applied, PS must be distributed into tissues or absorbed topically, getting in contact with cancerous or bacterial cells. Up to this point, PS remains inert but can be activated by light irradiation at a given wavelength to produce type I or type II ROS. Then, the aPDT will eliminate cancer or microbial cells through ROS formation and indirectly by stimulating the immune response [
13].
One limitation of the aPDT is that the PS is activated only in those places where light can be accessed on the surface or coatings of internal organs, which can be illuminated with probes. How much light penetrates living tissues will depend on its wavelength: a general rule for visible and NIR light says the shorter the wavelength (<600 nm), the less penetration; the longer the wavelength (>800 nm), the greater the penetration. Therefore, blue light penetrates poorly into the skin tissues, accessing only the dermis, while red light penetrates better into the dermis without even reaching the hypodermis. Infrared radiation, in theory, would penetrate the hypodermis [
21]. However, some lasers, such as erbium YAG or chromium YSGG, with wavelengths much higher than 800 nm (2940 and 2780 nm, respectively), show very low penetration capacities [
22]. Shorter wavelengths, however, are much more energetic than long wavelengths and, therefore, much more capable of activating PS molecules. Light ranges between 650–850 nm are considered the most suitable for aPDT; thus, PSs activated within these ranges have the most potential for clinical use. The strong activation produced by sorter wavelength light can be helpful for the aPDT treatment of superficial injuries, such as surgical wound infections. Also, PS activated at <600 nm could be beneficial in decontaminating surfaces or clinical materials [
23]. Other considerations must be taken when choosing a PS, such as its pharmacokinetics, which indicates that some accumulate in organs such as the liver, spleen, and kidneys [
24]. Also, the elimination half-life of PS ranges between 12 and 19 h, highlighting the need to take precautions due to the possible phototoxicity of sunlight [
25].
This scoping review aimed to conduct systematic research of evidence in this area to help researchers choose an aPDT appropriate to their needs and to summarize the development stage of aPDT applied to K. pneumoniae. The following research question was formulated: What is known from the literature about aPDT treatment of multidrug resistance K. pneumoniae infection, either in vitro or in vivo, and how many photosensitizers are used for this purpose?
2. Materials and Methods
Our methodology follows a protocol using the PRISMA extension for scoping reviews (PRISMA-ScR) guidelines, which is used to conduct a scoping review [
26]. This type of review was selected because it allows for a systematic review to synthesize literature evidence, provide an overview of the available research evidence, and elucidate potential gaps in the existing knowledge. The study has been registered on the Open Science Framework platform (Protocol Registration DOI:
https://doi.org/10.17605/OSF.IO/VKTDW).
2.1. Search Strategy and Eligibility Criteria
The search used a horizon of works no earlier than 2012; considering the PICO criterion, we agreed on 10 years and a buffer of 20%, 12 years old. Original articles were searched by FAF and ARB by consulting the PubMed (MESH), Google Scholar, and Scopus databases from January 2012 to September 2024. The search in these databases was carried out using the terms: “Klebsiella pneumoniae” AND “multidrug resistance” AND “photodynamic therapy” AND “coupled photosensitizer” OR “photosensitizer” AND “gram-negative” AND “ESKAPE”.
Studies were included if they meet: (1) original articles after 2012 referring to photodynamics associated with antimicrobial activity in K. pneumoniae in vitro and in vivo: clinical applications and synergism with antibiotics, other antimicrobial drugs, or PS coupled to other particles, (2) articles in English, (3) articles peer-reviewed. The exclusion criteria were: (1) Studies before 2012 or research not published in journals with an editorial board, (2) articles that were not accessed, (3) studies that did not declare the photosensitizer compound/concentration or light source/doses, (4) studies that included bacteria from the ESKAPE group but did not include K. pneumoniae, (5) studies without clinical significance (no significant K. pneumoniae growth reduction).
2.2. Information Sources and Search
All data were extracted solely from the databases mentioned above. In the Scopus database, in the Documents section, the Search within was “All fields”, and in the Search document, all terms mentioned above were added, one by one, in the given order. Then, the date ranged from “2012” to “Present” and Search. The “Article” button was selected in Document type, as well as “English” Language and “Final” Publication state. All open access was revised. In the first instance, keywords were searched in the title and abstract. The subsequent search was based on inclusion/exclusion criteria. Final documents were collected on EndNote 21. This information was used to eliminate duplicates.
2.3. Selection of Sources of Evidence and Data Charting Process
The articles were filtered by applying the abovementioned criteria in a PRISMA guideline that helped us better describe the systematic review (
Figure 2). The PRISMA criteria applied were as follows: Two researchers (ARB and FAF) conducted searches independently, collecting information according to previously assigned search criteria. Once each researcher obtained the results, they were pooled and compared to eliminate duplicates using EndNote 21 citation manager software. The most recent research was conducted on 4 October 2024. The articles found were read and filtered, applying the inclusion and exclusion criteria. The following relevant characteristics were extracted independently by two reviewers: (1) the names of authors; (2) the year of publication; (3) the aim of the study; (4) methods applied to analyze the aPDT treatment; (5) photosensitizer used mentioning doses; (6) light source and doses; (7) range of bacterial growth reduction from results; (8) present and possible future applications, and (9) the clinical importance of the findings.
2.4. Data Items and Synthesis of the Results
Two researchers (ARB and FAF) summarized and reviewed the data with the senior reviewer (Christian Erick Palavecino (CEP)). Data extracted were summarized in a table (
Table 1) and a narrative summary.