1. Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders in women of reproductive age, affecting approximately 6–15% of women worldwide depending on diagnostic criteria [
1,
2]. This condition not only significantly impacts reproductive health but also increases the risk of metabolic complications. Women with PCOS frequently exhibit metabolic disorders such as insulin resistance (IR), type 2 diabetes mellitus (T2DM), obesity, and metabolic syndrome (MetS). These metabolic disturbances contribute to an increased risk of cardiovascular disease (CVD), independent of body mass index (BMI). The association between PCOS and increased CVD risk is primarily attributed to abdominal fat accumulation and visceral adipose tissue dysfunction [
3,
4].
Traditionally, anthropometric measurements such as BMI, waist-to-hip ratio (WHR), and waist circumference (WC) have been used as surrogate markers for metabolic risk in PCOS. However, these measurements do not differentiate between subcutaneous and visceral fat, nor do they capture functional impairments in adipose tissue metabolism [
5]. Visceral adipose tissue dysfunction plays a central role in the development of IR, chronic low-grade inflammation, and cardiometabolic complications in PCOS patients. This limitation has led to the development of alternative metabolic indices that can more accurately reflect visceral adiposity and adipose tissue dysfunction [
6,
7].
The visceral adiposity index (VAI) and the dysfunctional adiposity index (DAI) are two recently proposed metabolic indices aimed at providing a more refined assessment of visceral fat accumulation and adipocyte dysfunction [
8]. Unlike BMI or WHR, these indices incorporate biochemical parameters, offering a more functional evaluation of metabolic health. The VAI is an established marker of abdominal obesity and IR, integrating WC, triglyceride (TG) levels, and high-density lipoprotein cholesterol (HDL-C) to predict metabolic risk. Similarly, the DAI has been developed as a more specific measure of adipose tissue dysfunction by combining WC, BMI, TG levels, and HDL-C [
9,
10,
11].
Emerging evidence suggests that VAI and DAI may provide better discrimination of metabolic risk in PCOS than traditional anthropometric measurements alone. However, their clinical utility in PCOS remains incompletely understood, particularly in relation to IR and MetS. Therefore, this study aimed to evaluate the predictive value of VAI and DAI for identifying IR and MetS in women with PCOS and to explore their potential role as practical, accessible, and objective biomarkers in clinical practice.
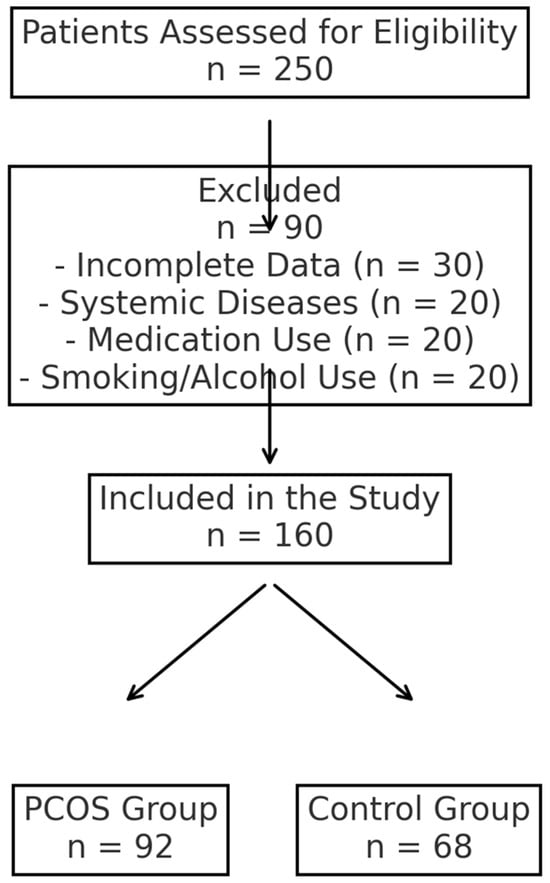
3. Results
The mean weight of women in the PCOS group was significantly higher than that of women in the control group (66.86 ± 15.94 vs. 62.11 ± 11.18,
p = 0.037). The average BMI and WC values of PCOS patients were also significantly higher compared to those in the control group (
p = 0.015 and
p = 0.034, respectively). The presence of insulin resistance (IR+) was detected at a statistically significantly higher rate in PCOS patients (
p < 0.001).
Table 1 presents the demographic and anthropometric values of both groups.
The levels of serum LH (
p = 0.013), E2 (
p = 0.029), total testosterone (
p < 0.001), FINS (
p < 0.001), TG (
p < 0.001), and HOMA-IR (
p < 0.001) were significantly higher in patients with PCOS compared to the control group. The FSH value in the PCOS group was significantly lower than that of the control group (5.59 (0.54–49.35) vs. 6.78 (3.12–16.83),
p < 0.001).
Table 2 provides a detailed comparison of biochemical parameters between the PCOS and control groups.
The VAI (3.43 (1.03–18.15) vs. 2.16 (0.65–10.60),
p = 0.003) and DAI (2.48 (0.72–10.05) vs. 1.54 (0.46–5.97),
p = 0.003) values were significantly higher in the PCOS group compared to the control group. The ideal cutoff value for the VAI in predicting the diagnosis of PCOS was 3.10, with a sensitivity of 56% and a specificity of 66%. The AUC for the VAI was 0.639 (
p = 0.001). The cutoff value for the DAI level was 0.22, with 54% sensitivity and 67% specificity, and an AUC of 0.635 (
p = 0.002). It should be noted that the VAI and DAI indices were not statistically significant for diagnosing PCOS.
Figure 2 presents the ROC curves for VAI and DAI in predicting a PCOS diagnosis.
Among PCOS patients diagnosed with MetS (MetS(+) PCOS), the VAI was significantly elevated compared to those without MetS (MetS(−) PCOS) (
p < 0.001). The optimal cutoff value for VAI in predicting a MetS diagnosis in PCOS was determined to be 4.73, demonstrating a sensitivity of 62% and a specificity of 92%. The AUC for VAI in the prediction of MetS in PCOS patients was 0.870 (
p < 0.001).
Figure 3 presents the ROC curves for VAI and DAI in predicting MetS in PCOS patients.
Additionally, the DAI values were significantly higher in MetS(+) PCOS patients compared to MetS(−) PCOS patients (p < 0.001). The optimal cutoff value for DAI was determined to be 2.44, yielding a sensitivity of 74% and a specificity of 80%. The AUC for DAI in the prediction of MetS in PCOS patients was 0.862 (p < 0.001).
The VAI was significantly elevated in PCOS patients with IR (IR(+) PCOS) compared to those without IR (IR(−) PCOS) (p < 0.001). The optimal cutoff value for VAI in identifying IR in PCOS patients was found to be 2.56, with a sensitivity of 82% and a specificity of 56%. The AUC for VAI was determined to be 0.754 in the prediction of IR in PCOS patients (p < 0.001).
Likewise, the DAI value was statistically significantly higher in IR(+) PCOS patients compared to IR(−) PCOS patients (p < 0.001). The cutoff value for DAI in determining IR in PCOS patients was established at 1.59, demonstrating a sensitivity of 82% and a specificity of 55%, with an AUC of 0.749 (p < 0.001).
4. Discussion
This study investigated the efficacy of novel metabolic indices, specifically the VAI and DAI, in predicting insulin resistance (IR) and metabolic syndrome (MetS) among women with PCOS. Furthermore, this research aimed to determine whether VAI and DAI could serve as reliable biomarkers for the diagnosis of PCOS. The results indicate that VAI and DAI do not demonstrate sufficient specificity or sensitivity for diagnosing PCOS. Nonetheless, our findings reveal that VAI and DAI may serve as robust markers for screening IR and MetS in this population. Although prior studies have examined the association of VAI with metabolic risk factors, therapeutic outcomes, and IR in PCOS patients, this study is the first to assess the relationship between DAI and both the diagnosis of PCOS and its association with IR and MetS [
19,
20,
21].
In our study, anthropometric measurements such as average weight (
p = 0.037), BMI (
p = 0.015), and WC (
p = 0.034) were found to be significantly higher in women with PCOS compared to healthy controls, consistent with previous studies. IR is recognized as a fundamental component of the pathophysiology of PCOS, and its effects are exacerbated by obesity [
22,
23]. Accordingly, our findings demonstrated that IR was detected at a statistically significantly higher rate in PCOS patients compared to controls (
p < 0.001). Similarly, MetS is a common metabolic complication among PCOS patients, as reflected in our study, where its prevalence was significantly higher in the PCOS group than in the control group (
p < 0.001) [
24].
Additionally, we observed that LH (
p = 0.013), E2 (
p = 0.029), total testosterone (
p < 0.001), FINS (
p < 0.001), TG (
p < 0.001), and VAI (
p = 0.003) were significantly elevated in the PCOS cohort. These findings align with other studies investigating biochemical parameter variations in PCOS [
25,
26]. Notably, this study is the first to assess DAI in PCOS, and it was found to be statistically significantly higher in the PCOS group compared to the control group (
p = 0.003).
It is well established that visceral adipose tissue is strongly correlated with metabolic risk factors and IR. Conventional anthropometric measurements, such as BMI and WC, are insufficient for accurately reflecting visceral fat distribution. Women diagnosed with PCOS exhibit a higher prevalence of central obesity and an increased risk of metabolic disturbances [
27,
28]. Discrepancies in findings may arise from methodological biases inherent in the varying measurement techniques of anthropometric indices. Furthermore, the pattern of adipose tissue distribution may differ significantly among PCOS patients with identical BMI values. Consequently, there is an urgent need to develop more specific indices that integrate anthropometric assessments with biochemical markers to accurately characterize visceral adiposity and its associated cardiometabolic complications, including IR and MetS, in individuals with PCOS [
29,
30].
The evidence indicates that VAI is superior to BMI in predicting IR and MetS. Oh et al. initially proposed that VAI could effectively replace visceral computed tomography as a marker for visceral adiposity, demonstrating its predictive capacity for IR in young women with PCOS [
31]. Visceral obesity affects 40–85% of women with PCOS, who also exhibit components of MetS, including IR, dyslipidemia, and hypertension. The VAI has emerged as a significant biomarker for the early detection of metabolic disorders in women with PCOS. However, a study conducted by Uysal et al. (2024) found no significant relationship between VAI values and IR(+) PCOS patients. Nonetheless, numerous studies, including ours, demonstrate that VAI is a strong indicator for identifying IR(+) and MetS(+) PCOS patients [
21].
The optimal cutoff value for VAI in predicting a MetS diagnosis in PCOS was determined to be 4.73, with an AUC of 0.870 in our study. Additionally, VAI was identified as a successful marker for predicting IR(+) PCOS patients, with an optimal cutoff of 2.56 and an AUC of 0.754. However, VAI is not a purely biochemical parameter; its geographic and racial variations due to the parameters used in its calculation, such as WC and BMI, may contribute to variability in study outcomes [
32].
DAI has been evaluated in a limited number of studies as a new marker reflecting adipocyte dysfunction. Reyes-Barrera et al. emphasized that DAI serves as a clinical surrogate for evaluating adipose tissue functionality and cardiometabolic health, reporting that DAI demonstrated good diagnostic values for detecting increased pericardial fat volume [
15]. Mantovani et al. found that in a population including both men and women, a DAI ≥ 1.065 was independently associated with diabetes, non-alcoholic fatty liver disease, subclinical atherosclerosis, and hypertension. They also noted that DAI is associated with early cardiometabolic abnormalities independent of adiposity and other risk factors [
33].
Although the lipid profile in PCOS patients was not drastically different from that in controls, it is crucial to consider that VAI and DAI incorporate additional metabolic parameters beyond lipid levels. The significant differences in waist circumference and BMI between groups suggest increased visceral adiposity in PCOS patients, which is a key driver of metabolic dysfunction. Furthermore, insulin resistance—a hallmark of PCOS—can lead to alterations in lipid metabolism and adipocyte function, even in the absence of overt dyslipidemia. Chronic low-grade inflammation and hormonal imbalances, particularly hyperinsulinemia and androgen excess, further contribute to adipose tissue dysfunction. These metabolic disturbances collectively explain why VAI and DAI remain elevated in PCOS patients despite a relatively similar lipid profile. This finding underscores the need for integrated metabolic indices that assess adipose dysfunction beyond conventional lipid measurements [
9,
25].
Given that DAI is a newly introduced clinical marker, previous studies have primarily focused on mixed-gender populations and have been conducted in Latin American and Hispanic communities [
15,
34]. In one study, 172,282 women were included, and DAI showed an AUC of 0.819 for MetS [
35]. Jalali et al. claimed that DAI was independently associated with IR and β-cell dysfunction in patients at high risk for T2D. However, in their study, 71.6% of the patients were women, and the cutoff values were not specified separately for men and women [
36].
Our study is the first to use DAI to predict MetS and IR positivity in PCOS patients. The optimal cutoff value for DAI was determined to be 2.44, with an AUC of 0.862 in predicting MetS in PCOS patients. The cutoff value for DAI in determining IR in PCOS patients was established at 1.59, with an AUC of 0.749 in our study.
This study has several limitations. First, the cross-sectional design prevents causal inferences regarding the relationships between VAI, DAI, and metabolic disorders in PCOS. Second, this study was conducted at a single center, which may limit its generalizability to broader populations. Third, important confounding factors such as physical activity, dietary intake, and socioeconomic status were not assessed, which could have influenced the findings. Finally, although our study provides valuable insights into the role of VAI and DAI in PCOS, further large-scale, multicenter, prospective studies are necessary to validate these findings and determine the optimal cutoff values for different populations.